Tuesday Poster Session
Category: Practice Management
P4929 - Bridging Healthcare Gaps: Improving Access to Gastroenterology Services in Hard-to-Reach Areas Using an Integrated Care Approach
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Adebolanle Ayinde, MD, MPH
CHRISTUS Health | Texas A&M School of Medicine
Longview, TX
Presenting Author(s)
Award: Presidential Poster Award
Adebolanle Ayinde, MD, MPH1, Ifeoluwa C. Daramola, BSc, MPH, MD2, Oluwatayo J. Awolumate, MD3, Adedeji Adenusi, MD, MPH4, Joshua Eyitemi, MD, MPH, MS5
1CHRISTUS Health | Texas A&M School of Medicine, Longview, TX; 2Cypress Internal Medicine, Swift Current, SK, Canada; 3Howard University Hospital, Washington, DC; 4One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 5Saskatchewan Health Authority, Swift Current, SK, Canada
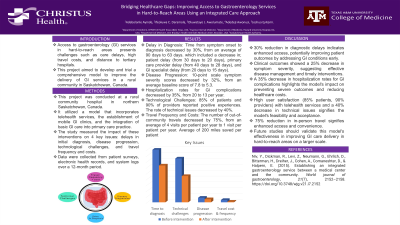
Introduction: Access to gastroenterology (GI) services in hard-to-reach areas presents challenges such as care delays, high travel costs, and distance to tertiary hospitals. This project aimed to develop and trial a comprehensive model to improve the delivery of GI services in a rural community in Saskatchewan, Canada.
Methods: This project was conducted at a rural community hospital in northern Saskatchewan, Canada. It utilized a model that incorporates telehealth services, the establishment of mobile GI clinics, and the integration of basic GI care into primary care practice. The study measured the impact of these interventions on 4 key issues: delays in initial diagnosis, disease progression, technological challenges, and travel frequency and costs. Data were collected from patient surveys, electronic health records, and system logs over a 12-month period.
Results: Delay in Diagnosis: Time from symptom onset to diagnosis decreased by 30%, from an average of 90 days to 63 days. This included a decrease in; patient delay (from 30 days to 20 days), primary care provider delay (from 40 days to 28 days), and GI specialist delay (from 20 days to 15 days).Disease Progression: On a 10-point scale, symptom severity scores decreased by 32%, from an average baseline score of 7.8 to 5.3. Hospitalization rates for GI complications decreased by 35%, from 20 to 13 per year. Technological Challenges: 85% of patients and 90% of providers reported positive experiences. The rate of technical issues decreased by 40%. Travel Frequency and Costs: The number of out-of-community travels decreased by 75%, from an average of 4 visits per patient per year to 1 visit per patient per year. On average, patients saved 200 miles per year in travel distance.
Discussion: A 30% reduction in diagnostic delays indicates enhanced access, potentially improving patient outcomes by addressing GI conditions early. Clinical outcomes showed a 25% decrease in symptom severity, suggesting effective disease management and timely interventions. A 35% decrease in hospitalization rates for GI complications highlights the model's impact on preventing severe outcomes and reducing healthcare costs. High user satisfaction (85% patients, 90% providers) with telehealth services and a 40% decrease in technical issues signifies the model's feasibility and acceptance. The 75% reduction in in-person travel signifies enhanced access and convenience. Future studies should validate this model's effectiveness in improving GI care delivery in larger settings.
Disclosures:
Adebolanle Ayinde, MD, MPH1, Ifeoluwa C. Daramola, BSc, MPH, MD2, Oluwatayo J. Awolumate, MD3, Adedeji Adenusi, MD, MPH4, Joshua Eyitemi, MD, MPH, MS5. P4929 - Bridging Healthcare Gaps: Improving Access to Gastroenterology Services in Hard-to-Reach Areas Using an Integrated Care Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Adebolanle Ayinde, MD, MPH1, Ifeoluwa C. Daramola, BSc, MPH, MD2, Oluwatayo J. Awolumate, MD3, Adedeji Adenusi, MD, MPH4, Joshua Eyitemi, MD, MPH, MS5
1CHRISTUS Health | Texas A&M School of Medicine, Longview, TX; 2Cypress Internal Medicine, Swift Current, SK, Canada; 3Howard University Hospital, Washington, DC; 4One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 5Saskatchewan Health Authority, Swift Current, SK, Canada
Introduction: Access to gastroenterology (GI) services in hard-to-reach areas presents challenges such as care delays, high travel costs, and distance to tertiary hospitals. This project aimed to develop and trial a comprehensive model to improve the delivery of GI services in a rural community in Saskatchewan, Canada.
Methods: This project was conducted at a rural community hospital in northern Saskatchewan, Canada. It utilized a model that incorporates telehealth services, the establishment of mobile GI clinics, and the integration of basic GI care into primary care practice. The study measured the impact of these interventions on 4 key issues: delays in initial diagnosis, disease progression, technological challenges, and travel frequency and costs. Data were collected from patient surveys, electronic health records, and system logs over a 12-month period.
Results: Delay in Diagnosis: Time from symptom onset to diagnosis decreased by 30%, from an average of 90 days to 63 days. This included a decrease in; patient delay (from 30 days to 20 days), primary care provider delay (from 40 days to 28 days), and GI specialist delay (from 20 days to 15 days).Disease Progression: On a 10-point scale, symptom severity scores decreased by 32%, from an average baseline score of 7.8 to 5.3. Hospitalization rates for GI complications decreased by 35%, from 20 to 13 per year. Technological Challenges: 85% of patients and 90% of providers reported positive experiences. The rate of technical issues decreased by 40%. Travel Frequency and Costs: The number of out-of-community travels decreased by 75%, from an average of 4 visits per patient per year to 1 visit per patient per year. On average, patients saved 200 miles per year in travel distance.
Discussion: A 30% reduction in diagnostic delays indicates enhanced access, potentially improving patient outcomes by addressing GI conditions early. Clinical outcomes showed a 25% decrease in symptom severity, suggesting effective disease management and timely interventions. A 35% decrease in hospitalization rates for GI complications highlights the model's impact on preventing severe outcomes and reducing healthcare costs. High user satisfaction (85% patients, 90% providers) with telehealth services and a 40% decrease in technical issues signifies the model's feasibility and acceptance. The 75% reduction in in-person travel signifies enhanced access and convenience. Future studies should validate this model's effectiveness in improving GI care delivery in larger settings.
Disclosures:
Adebolanle Ayinde indicated no relevant financial relationships.
Ifeoluwa Daramola indicated no relevant financial relationships.
Oluwatayo Awolumate indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Joshua Eyitemi indicated no relevant financial relationships.
Adebolanle Ayinde, MD, MPH1, Ifeoluwa C. Daramola, BSc, MPH, MD2, Oluwatayo J. Awolumate, MD3, Adedeji Adenusi, MD, MPH4, Joshua Eyitemi, MD, MPH, MS5. P4929 - Bridging Healthcare Gaps: Improving Access to Gastroenterology Services in Hard-to-Reach Areas Using an Integrated Care Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

