Tuesday Poster Session
Category: Small Intestine
P4932 - Celiac Disease and Inflammatory Bowel Disease: Characteristics of a Dual Diagnosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Alexandria Markley, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Alexandria Markley, MD1, Luis Rendon, MD2, Carlos Diola, MD3, Yontan Israel, MD3, Haley Waite, MS4, Peter Green, MD5, Christopher Cao, MD3
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY; 4Mount Sinai Health System, New York, NY; 5New York-Presbyterian/Columbia University Irving Medical Center, New York, NY
Introduction: A bidirectional association of celiac disease (CeD) and inflammatory bowel disease (IBD) has been well established. The existence of this dual diagnosis (CeD-IBD) poses questions regarding diagnosis, treatment, and potential synergistic effects on disease course. There remains a need for further understanding of the clinical implications of this dual diagnosis.
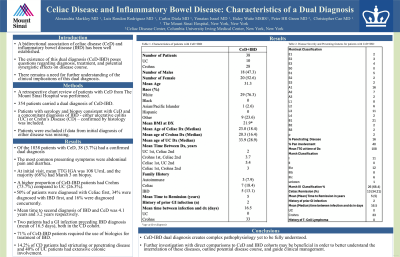
Methods: A retrospective chart review of patients with CeD from The Mount Sinai Hospital was performed. In total, 354 patients carried a dual diagnosis of CeD-IBD. Any individual with serology and biopsy consistent with CeD and a concomitant diagnosis of IBD - either ulcerative colitis (UC) or Crohn’s Disease (CD) – confirmed by histology was included. Patients were excluded if data from initial diagnosis of either disease was missing.
Results: Of the 1038 patients with CeD, a total of 38 (3.7%) carried a confirmed dual diagnosis – 53% were female and mean age of the cohort was 31.29. The most common presenting symptoms were abdominal pain and diarrhea. At initial visit, mean TTG IGA was 108 U/mL and the majority (68%) had Marsh 3 on biopsy. Mean age of diagnosis was oldest in the CeD-UC cohort. A higher proportion of CeD-IBD patients had Crohns (73.7%) compared to UC (26.3%). Interval time to second diagnosis of IBD and CeD was 4.1 years and 3.2 years respectively. Two patients had a GI infection preceding IBD diagnosis (mean interval of 16.5 days), both in the CD cohort. 71% of CeD-IBD patients required the use of biologics for treatment of IBD. 14.2% of CD patients had stricturing or penetrating disease and 40% of UC patients had extensive colonic involvement.
Discussion: CeD-IBD dual diagnosis creates complex pathophysiology yet to be fully understood. Further investigation with direct comparisons to CeD and IBD cohorts may be beneficial in order to better understand the interrelation of these diseases, outline potential disease course, and guide clinical management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexandria Markley, MD1, Luis Rendon, MD2, Carlos Diola, MD3, Yontan Israel, MD3, Haley Waite, MS4, Peter Green, MD5, Christopher Cao, MD3. P4932 - Celiac Disease and Inflammatory Bowel Disease: Characteristics of a Dual Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY; 4Mount Sinai Health System, New York, NY; 5New York-Presbyterian/Columbia University Irving Medical Center, New York, NY
Introduction: A bidirectional association of celiac disease (CeD) and inflammatory bowel disease (IBD) has been well established. The existence of this dual diagnosis (CeD-IBD) poses questions regarding diagnosis, treatment, and potential synergistic effects on disease course. There remains a need for further understanding of the clinical implications of this dual diagnosis.
Methods: A retrospective chart review of patients with CeD from The Mount Sinai Hospital was performed. In total, 354 patients carried a dual diagnosis of CeD-IBD. Any individual with serology and biopsy consistent with CeD and a concomitant diagnosis of IBD - either ulcerative colitis (UC) or Crohn’s Disease (CD) – confirmed by histology was included. Patients were excluded if data from initial diagnosis of either disease was missing.
Results: Of the 1038 patients with CeD, a total of 38 (3.7%) carried a confirmed dual diagnosis – 53% were female and mean age of the cohort was 31.29. The most common presenting symptoms were abdominal pain and diarrhea. At initial visit, mean TTG IGA was 108 U/mL and the majority (68%) had Marsh 3 on biopsy. Mean age of diagnosis was oldest in the CeD-UC cohort. A higher proportion of CeD-IBD patients had Crohns (73.7%) compared to UC (26.3%). Interval time to second diagnosis of IBD and CeD was 4.1 years and 3.2 years respectively. Two patients had a GI infection preceding IBD diagnosis (mean interval of 16.5 days), both in the CD cohort. 71% of CeD-IBD patients required the use of biologics for treatment of IBD. 14.2% of CD patients had stricturing or penetrating disease and 40% of UC patients had extensive colonic involvement.
Discussion: CeD-IBD dual diagnosis creates complex pathophysiology yet to be fully understood. Further investigation with direct comparisons to CeD and IBD cohorts may be beneficial in order to better understand the interrelation of these diseases, outline potential disease course, and guide clinical management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexandria Markley indicated no relevant financial relationships.
Luis Rendon indicated no relevant financial relationships.
Carlos Diola indicated no relevant financial relationships.
Yontan Israel indicated no relevant financial relationships.
Haley Waite indicated no relevant financial relationships.
Peter Green indicated no relevant financial relationships.
Christopher Cao indicated no relevant financial relationships.
Alexandria Markley, MD1, Luis Rendon, MD2, Carlos Diola, MD3, Yontan Israel, MD3, Haley Waite, MS4, Peter Green, MD5, Christopher Cao, MD3. P4932 - Celiac Disease and Inflammatory Bowel Disease: Characteristics of a Dual Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
