Tuesday Poster Session
Category: Small Intestine
P4943 - When Celiac Disease Becomes a Crisis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JL
Jean Lafontant, MD, MPH
University of Rochester Medical Center
Rochester, NY
Presenting Author(s)
Jean Lafontant, MD, MPH, Timothy J. Lee, MD, Natalie Mitchell, MD, Nicholas Bartell, MD, Maisa Abdalla, MD, MPH
University of Rochester Medical Center, Rochester, NY
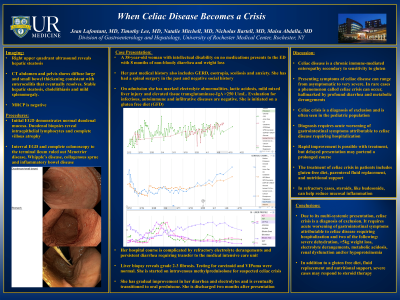
Introduction: Celiac disease (CD) is a chronic immune-mediated enteropathy secondary to sensitivity to gluten. Presenting symptoms of CD can range from asymptomatic to very severe in a rare phenomenon called celiac crisis (CC), hallmarked by profound diarrhea and metabolic derangements.
Case Description/Methods: A 38-year-old woman with intellectual disability on no medications presented with chronic non-bloody diarrhea with weight loss. On admission, she had marked electrolyte abnormalities and mild mixed liver injury. A broad evaluation for her diarrhea was unrevealing, including normal thyroid function testing, infectious stool studies, fecal elastase, fecal calprotectin and stool alpha 1 antitrypsin. Her labs were notable for an elevated tissue transglutaminase-IgA >250 U/mL. Initial EGD demonstrated normal duodenal mucosa; however, duodenal biopsies revealed intraepithelial lymphocytes and complete villous atrophy. She was initiated on a gluten free diet (GFD).
Regarding her mixed liver injury, right upper quadrant ultrasound revealed hepatic steatosis. Evaluation for viral hepatidities, autoimmune and infiltrative diseases were normal. Given persistent liver enzyme elevation and critical illness, the patient underwent a liver biopsy, which demonstrated steatohepatitis and grade 2-3 fibrosis thought to be secondary to CD.
Her hospital course was complicated by refractory electrolyte derangements and persistent diarrhea requiring transfer to the medical intensive care unit. Testing for carcinoid and VIPoma was normal. Interval EGD and complete colonoscopy to the terminal ileum ruled out Menetrier disease, Whipple’s disease, collagenous sprue and inflammatory bowel disease. She was started on intravenous methylprednisolone for suspected CC with gradual improvement in her weight, diarrhea, electrolytes and liver enzymes. The patient was transitioned to oral prednisone with plans for outpatient taper.
Discussion: CC is a diagnosis of exclusion and is often seen in the pediatric population. Diagnosis requires acute worsening of GI symptoms attributable to CD requiring hospitalization and two of the following: severe dehydration, >5kg weight loss, electrolyte derangements, metabolic acidosis, renal dysfunction or hypoproteinemia. In addition to a GFD and nutrition support, severe cases may respond to steroid therapy. Rapid improvement is possible with treatment, but delayed presentation may portend a prolonged course.
Disclosures:
Jean Lafontant, MD, MPH, Timothy J. Lee, MD, Natalie Mitchell, MD, Nicholas Bartell, MD, Maisa Abdalla, MD, MPH. P4943 - When Celiac Disease Becomes a Crisis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Rochester Medical Center, Rochester, NY
Introduction: Celiac disease (CD) is a chronic immune-mediated enteropathy secondary to sensitivity to gluten. Presenting symptoms of CD can range from asymptomatic to very severe in a rare phenomenon called celiac crisis (CC), hallmarked by profound diarrhea and metabolic derangements.
Case Description/Methods: A 38-year-old woman with intellectual disability on no medications presented with chronic non-bloody diarrhea with weight loss. On admission, she had marked electrolyte abnormalities and mild mixed liver injury. A broad evaluation for her diarrhea was unrevealing, including normal thyroid function testing, infectious stool studies, fecal elastase, fecal calprotectin and stool alpha 1 antitrypsin. Her labs were notable for an elevated tissue transglutaminase-IgA >250 U/mL. Initial EGD demonstrated normal duodenal mucosa; however, duodenal biopsies revealed intraepithelial lymphocytes and complete villous atrophy. She was initiated on a gluten free diet (GFD).
Regarding her mixed liver injury, right upper quadrant ultrasound revealed hepatic steatosis. Evaluation for viral hepatidities, autoimmune and infiltrative diseases were normal. Given persistent liver enzyme elevation and critical illness, the patient underwent a liver biopsy, which demonstrated steatohepatitis and grade 2-3 fibrosis thought to be secondary to CD.
Her hospital course was complicated by refractory electrolyte derangements and persistent diarrhea requiring transfer to the medical intensive care unit. Testing for carcinoid and VIPoma was normal. Interval EGD and complete colonoscopy to the terminal ileum ruled out Menetrier disease, Whipple’s disease, collagenous sprue and inflammatory bowel disease. She was started on intravenous methylprednisolone for suspected CC with gradual improvement in her weight, diarrhea, electrolytes and liver enzymes. The patient was transitioned to oral prednisone with plans for outpatient taper.
Discussion: CC is a diagnosis of exclusion and is often seen in the pediatric population. Diagnosis requires acute worsening of GI symptoms attributable to CD requiring hospitalization and two of the following: severe dehydration, >5kg weight loss, electrolyte derangements, metabolic acidosis, renal dysfunction or hypoproteinemia. In addition to a GFD and nutrition support, severe cases may respond to steroid therapy. Rapid improvement is possible with treatment, but delayed presentation may portend a prolonged course.
Disclosures:
Jean Lafontant indicated no relevant financial relationships.
Timothy Lee indicated no relevant financial relationships.
Natalie Mitchell indicated no relevant financial relationships.
Nicholas Bartell indicated no relevant financial relationships.
Maisa Abdalla indicated no relevant financial relationships.
Jean Lafontant, MD, MPH, Timothy J. Lee, MD, Natalie Mitchell, MD, Nicholas Bartell, MD, Maisa Abdalla, MD, MPH. P4943 - When Celiac Disease Becomes a Crisis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
