Tuesday Poster Session
Category: Small Intestine
P4956 - Plasmablastic Lymphoma of the Small Bowel and Appendix Complicated by Perforation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zahra Dossaji, DO
Kirk Kerkorian School of Medicine at the University of Nevada
Las Vegas, NV
Presenting Author(s)
Zahra Dossaji, DO, Adam Khattak, DO, Amith Subhash, MD, Shahid Wahid, MD
Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV
Introduction: Plasmablastic lymphoma (PBL) is a rare, aggressive subtype of diffuse large B-cell lymphoma associated with immunosuppression, commonly seen in patients with HIV/AIDS, post-solid organ transplantation, or steroid hormone use. PBL accounts for about 11% of AIDS-related lymphomas and is characterized by immunoblastic morphology with plasma cell markers. Up to 70% of cases are associated with Epstein-Barr virus (EBV) co-infection. PBL typically presents as a mass in extra-nodal sites, usually in the oral cavity or gastrointestinal tract. This is the first reported case of PBL presenting as an appendiceal orifice lesion.
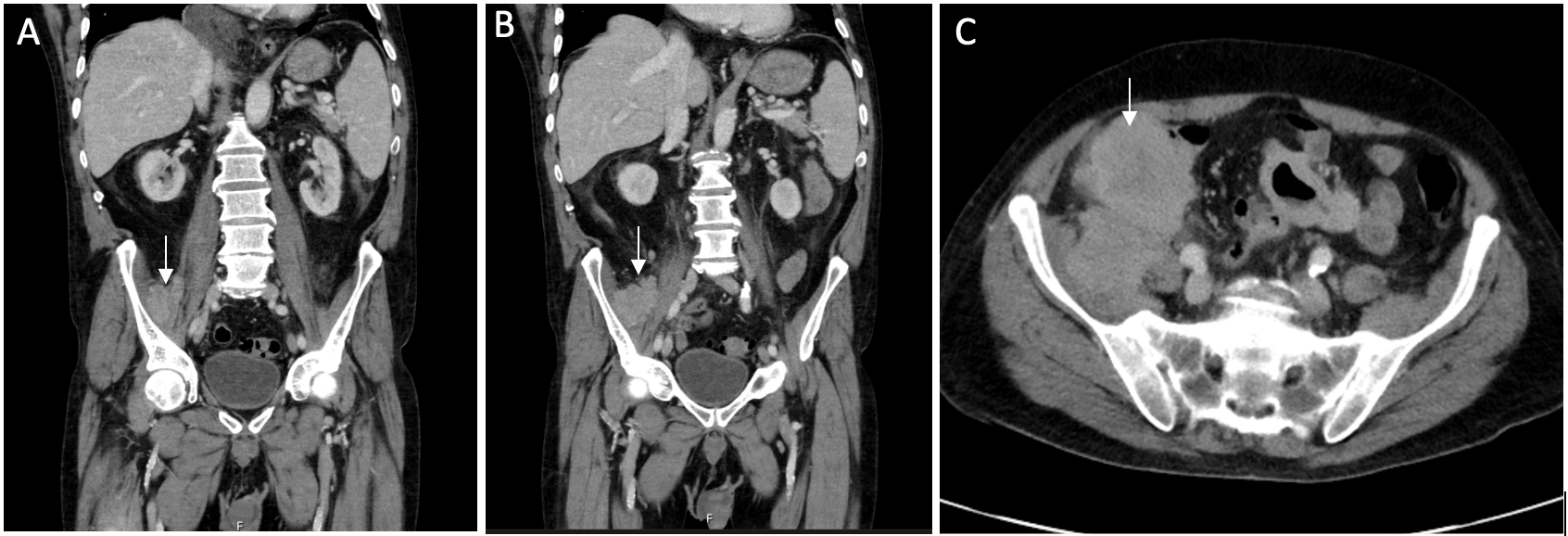
Case Description/Methods: A 64-year-old male with an undetectable HIV load and a normal CD4 count on Biktarvy presented to the emergency room with melena and symptomatic hypotension. His workup showed microcytic anemia (Hgb 6.3 g/dL, MCV 80 fL). Diagnostic endoscopy and colonoscopy revealed significant periappendiceal edema and a nodular mucosal lesion on the appendiceal orifice, which was biopsied. The remainder of the colonoscopy was unremarkable. A follow-up CT of the abdomen and pelvis with IV contrast revealed a large cecal mass measuring 7.2 cm x 6.9 cm, extending into the right psoas muscle. Forty-eight hours after the colonoscopy, the patient developed acute abdominal pain, and a repeat CT revealed a new pneumoperitoneum surrounding the liver and bowel and a re-demonstration of the mass with internal foci of gas. He underwent emergency surgery and was found to have a perforated mass in the ileum. A resection of the jejunal and ileal mass was performed, along with primary anastomoses. Final biopsies of the appendiceal lesion, ileum, and jejunum mass showed positive staining for CD43, CD45, CD10, and EBV, supporting a diagnosis of PBL.
Discussion: PBL is a rare, highly aggressive lymphoma often seen in HIV-positive patients despite virological suppression. Due to its rarity, there is no accepted evidence-based therapy, and chemotherapy remains the first-line treatment. Most patients achieve complete remission, but many relapse, with a median progression-free survival of six months and an overall median survival of 11-13 months. Without chemotherapy, survival is around three months. Given the poor prognosis, we recommend considering PBL for early identification and management in HIV-positive patients presenting with anemia and melena and referring these patients for abdominal imaging and urgent endoscopy.
Disclosures:
Zahra Dossaji, DO, Adam Khattak, DO, Amith Subhash, MD, Shahid Wahid, MD. P4956 - Plasmablastic Lymphoma of the Small Bowel and Appendix Complicated by Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV
Introduction: Plasmablastic lymphoma (PBL) is a rare, aggressive subtype of diffuse large B-cell lymphoma associated with immunosuppression, commonly seen in patients with HIV/AIDS, post-solid organ transplantation, or steroid hormone use. PBL accounts for about 11% of AIDS-related lymphomas and is characterized by immunoblastic morphology with plasma cell markers. Up to 70% of cases are associated with Epstein-Barr virus (EBV) co-infection. PBL typically presents as a mass in extra-nodal sites, usually in the oral cavity or gastrointestinal tract. This is the first reported case of PBL presenting as an appendiceal orifice lesion.
Case Description/Methods: A 64-year-old male with an undetectable HIV load and a normal CD4 count on Biktarvy presented to the emergency room with melena and symptomatic hypotension. His workup showed microcytic anemia (Hgb 6.3 g/dL, MCV 80 fL). Diagnostic endoscopy and colonoscopy revealed significant periappendiceal edema and a nodular mucosal lesion on the appendiceal orifice, which was biopsied. The remainder of the colonoscopy was unremarkable. A follow-up CT of the abdomen and pelvis with IV contrast revealed a large cecal mass measuring 7.2 cm x 6.9 cm, extending into the right psoas muscle. Forty-eight hours after the colonoscopy, the patient developed acute abdominal pain, and a repeat CT revealed a new pneumoperitoneum surrounding the liver and bowel and a re-demonstration of the mass with internal foci of gas. He underwent emergency surgery and was found to have a perforated mass in the ileum. A resection of the jejunal and ileal mass was performed, along with primary anastomoses. Final biopsies of the appendiceal lesion, ileum, and jejunum mass showed positive staining for CD43, CD45, CD10, and EBV, supporting a diagnosis of PBL.
Discussion: PBL is a rare, highly aggressive lymphoma often seen in HIV-positive patients despite virological suppression. Due to its rarity, there is no accepted evidence-based therapy, and chemotherapy remains the first-line treatment. Most patients achieve complete remission, but many relapse, with a median progression-free survival of six months and an overall median survival of 11-13 months. Without chemotherapy, survival is around three months. Given the poor prognosis, we recommend considering PBL for early identification and management in HIV-positive patients presenting with anemia and melena and referring these patients for abdominal imaging and urgent endoscopy.
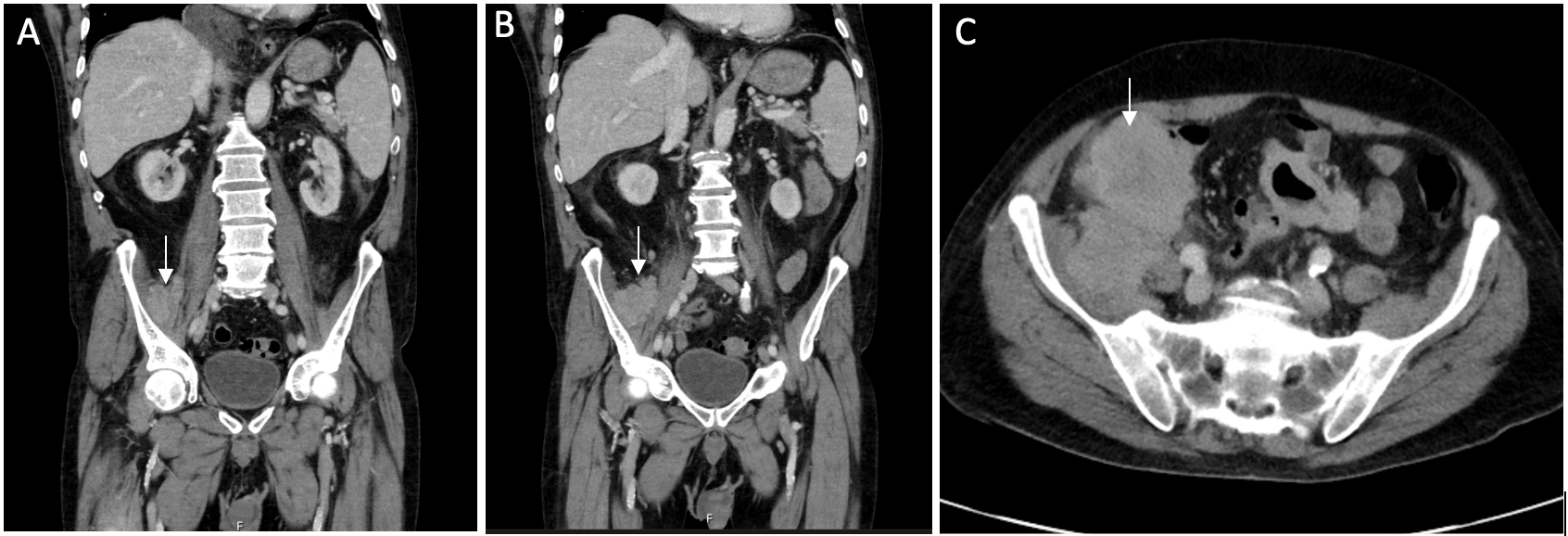
Figure: A, B, C) The arrow indicates a large heterogeneous mass in the area of the cecum, extending beyond the wall to involve the right iliopsoas muscle.
Disclosures:
Zahra Dossaji indicated no relevant financial relationships.
Adam Khattak indicated no relevant financial relationships.
Amith Subhash indicated no relevant financial relationships.
Shahid Wahid indicated no relevant financial relationships.
Zahra Dossaji, DO, Adam Khattak, DO, Amith Subhash, MD, Shahid Wahid, MD. P4956 - Plasmablastic Lymphoma of the Small Bowel and Appendix Complicated by Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
