Tuesday Poster Session
Category: Small Intestine
P4971 - More Than Skin Deep: Symptomatic Metastatic Melanoma in the Small Bowel
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Ayeetin Azah, MD, MBA
Walter Reed National Military Medical Center
Gaithersburg, MD
Presenting Author(s)
Ayeetin Azah, MD, MBA1, Azfar S. Syed, DO, MBA2, Patrick Young, MD2
1Walter Reed National Military Medical Center, Gaithersburg, MD; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Melanoma is the third most common skin cancer, but metastatic melanoma (MM) accounts for only 4% of cases. Only 1-5% of MM cases GI tract (GIT) metastases present symptomatically. Symptoms tend to be nonspecific such as abdominal pain, constipation, weight loss, and fatigue. We report a case of a patient diagnosed with small intestinal MM discovered during the evaluation of iron deficiency anemia.
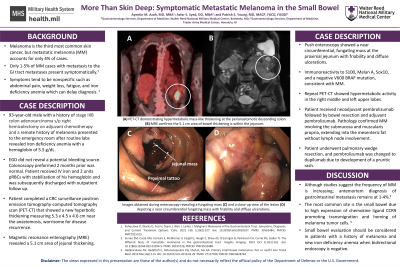
Case Description/Methods: A 93-year-old male with a history of stage III colon adenocarcinoma s/p right hemicolectomy on adjuvant chemotherapy and a remote history of melanoma presented to the emergency room after routine labs revealed iron deficiency anemia with a hemoglobin (Hb) of 5.5 g/dL. He denied bleeding and esophagogastroduodenoscopy did not reveal a potential bleeding source. Colonoscopy performed 2 months prior was normal. He received intravenous iron and 2 units of packed red blood cells with stabilization of Hb and was discharged to complete a surveillance positron emission tomography-computed tomography scan (PET-CT). This scan showed a new hypermetabolic thickening near the anastomosis, worrisome for disease recurrence. Given his advanced age, he underwent magnetic resonance enterography which revealed a 5.1 cm area of jejunal thickening. Push enteroscopy showed a near circumferential, fungating, proximal jejunal mass with friability and diffuse ulcerations. Biopsies revealed immunoreactivity to S100, Melan A, Sox10, and a negative V600 BRAF mutation, consistent with MM. Repeat PET-CT showed hypermetabolic activity in the right middle and left upper lung lobes. The patient received neoadjuvant pembrolizumab followed by bowel resection and adjuvant pembrolizumab. Pathology confirmed MM involving the submucosa and muscularis propria, extending to the mesenteric fat without evidence of lymph node involvement. He underwent pulmonary wedge resection, and pembrolizumab was changed to dupilumab due to development of a pruritic rash.
Discussion: Although studies suggest the frequency of MM is increasing, antemortem diagnosis of GIT metastasis remains quite rare with a detection rate as low as 2%. In a patient with a history of melanoma and new iron deficiency anemia, one should consider small intestinal evaluation with advanced imaging or direct visualization when bidirectional endoscopy is negative, due to the potential for GIT MM.
Disclaimer: The views expressed are those of the authors and do not reflect the official policy of the Department of Defense or U.S. Government.
Disclosures:
Ayeetin Azah, MD, MBA1, Azfar S. Syed, DO, MBA2, Patrick Young, MD2. P4971 - More Than Skin Deep: Symptomatic Metastatic Melanoma in the Small Bowel, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Gaithersburg, MD; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Melanoma is the third most common skin cancer, but metastatic melanoma (MM) accounts for only 4% of cases. Only 1-5% of MM cases GI tract (GIT) metastases present symptomatically. Symptoms tend to be nonspecific such as abdominal pain, constipation, weight loss, and fatigue. We report a case of a patient diagnosed with small intestinal MM discovered during the evaluation of iron deficiency anemia.
Case Description/Methods: A 93-year-old male with a history of stage III colon adenocarcinoma s/p right hemicolectomy on adjuvant chemotherapy and a remote history of melanoma presented to the emergency room after routine labs revealed iron deficiency anemia with a hemoglobin (Hb) of 5.5 g/dL. He denied bleeding and esophagogastroduodenoscopy did not reveal a potential bleeding source. Colonoscopy performed 2 months prior was normal. He received intravenous iron and 2 units of packed red blood cells with stabilization of Hb and was discharged to complete a surveillance positron emission tomography-computed tomography scan (PET-CT). This scan showed a new hypermetabolic thickening near the anastomosis, worrisome for disease recurrence. Given his advanced age, he underwent magnetic resonance enterography which revealed a 5.1 cm area of jejunal thickening. Push enteroscopy showed a near circumferential, fungating, proximal jejunal mass with friability and diffuse ulcerations. Biopsies revealed immunoreactivity to S100, Melan A, Sox10, and a negative V600 BRAF mutation, consistent with MM. Repeat PET-CT showed hypermetabolic activity in the right middle and left upper lung lobes. The patient received neoadjuvant pembrolizumab followed by bowel resection and adjuvant pembrolizumab. Pathology confirmed MM involving the submucosa and muscularis propria, extending to the mesenteric fat without evidence of lymph node involvement. He underwent pulmonary wedge resection, and pembrolizumab was changed to dupilumab due to development of a pruritic rash.
Discussion: Although studies suggest the frequency of MM is increasing, antemortem diagnosis of GIT metastasis remains quite rare with a detection rate as low as 2%. In a patient with a history of melanoma and new iron deficiency anemia, one should consider small intestinal evaluation with advanced imaging or direct visualization when bidirectional endoscopy is negative, due to the potential for GIT MM.
Disclaimer: The views expressed are those of the authors and do not reflect the official policy of the Department of Defense or U.S. Government.
Disclosures:
Ayeetin Azah indicated no relevant financial relationships.
Azfar Syed indicated no relevant financial relationships.
Patrick Young: Elements Endoscopy – Consultant.
Ayeetin Azah, MD, MBA1, Azfar S. Syed, DO, MBA2, Patrick Young, MD2. P4971 - More Than Skin Deep: Symptomatic Metastatic Melanoma in the Small Bowel, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
