Tuesday Poster Session
Category: Small Intestine
P4979 - Gastroenterologist's Recognition of Rare Adverse Drug Effect Prevents Further Harm in a Patient with Small Bowel Obstruction Due to Lisinopril: A Case Report and Literature Review
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Essam Rashad, MBBCh
Parkview Medical Center
Fort Wayne, IN
Presenting Author(s)
Essam Rashad, MBBCh1, Soukaina El Yazal, MD2
1Parkview Medical Center, Fort Wayne, IN; 2Ministry of Health, Zagora, Souss-Massa-Dr, Morocco
Introduction: Angiotensin-converting enzyme (ACE) inhibitors are widely prescribed for hypertension and heart failure but can cause angioedema by increasing bradykinin levels. Though rare, ACE inhibitor-induced angioedema can affect the bowel, leading to severe gastrointestinal symptoms. This case report details a 41-year-old female who developed recurrent bowel obstruction following the initiation of lisinopril-hydrochlorothiazide, necessitating multiple hospitalizations and diagnostic laparoscopy, illustrating the diagnostic challenges and the need for clinician awareness of this adverse effect. A literature review accompanies the case, summarizing the epidemiology, clinical manifestations, and outcomes of this condition.
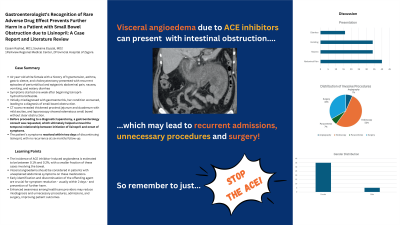
Case Description/Methods: A 41-year-old white female with a history of hypertension, asthma, gastric sleeve, and cholecystectomy presented with recurrent episodes of periumbilical and epigastric abdominal pain, nausea, vomiting, and watery diarrhea starting one week after beginning lisinopril-hydrochlorothiazide. Initially misdiagnosed with gastroenteritis, her condition worsened, leading to a diagnosis of small bowel obstruction. CT scans revealed thickened proximal jejunum and duodenum with mild ascites, and laparoscopy showed edematous small bowel without clear obstruction. The patient’s symptoms resolved within two days of discontinuing lisinopril, with no recurrence at six months follow-up.
Discussion: Visceral angioedema due to ACE inhibitors, while rare, should be considered in patients with unexplained abdominal symptoms on these medications. We conducted a literature review of 35 published case reports exhibiting 40 patients diagnosed with visceral angioedema due to ACE inhibitor therapy. The condition predominantly affects females (35/40). Symptoms consisted of abdominal pain, nausea, vomiting and/or diarrhea, and began from 12 hours to 15 years after initiation of the drug; lisinopril was the most common offending agent (28/40). Imaging usually shows bowel wall thickening and edema. Diagnosis is often delayed, leading to invasive investigations including angiography (1/40), endoscopy (8/40), paracentesis (1/40), and surgery (5/40). The primary treatment is the cessation of the offending drug, which often leads to symptom resolution within 72 hours. This case highlights the importance of recognizing ACE inhibitor-associated angioedema to avoid unnecessary surgical interventions and prevent serious complications.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Essam Rashad, MBBCh1, Soukaina El Yazal, MD2. P4979 - Gastroenterologist's Recognition of Rare Adverse Drug Effect Prevents Further Harm in a Patient with Small Bowel Obstruction Due to Lisinopril: A Case Report and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Parkview Medical Center, Fort Wayne, IN; 2Ministry of Health, Zagora, Souss-Massa-Dr, Morocco
Introduction: Angiotensin-converting enzyme (ACE) inhibitors are widely prescribed for hypertension and heart failure but can cause angioedema by increasing bradykinin levels. Though rare, ACE inhibitor-induced angioedema can affect the bowel, leading to severe gastrointestinal symptoms. This case report details a 41-year-old female who developed recurrent bowel obstruction following the initiation of lisinopril-hydrochlorothiazide, necessitating multiple hospitalizations and diagnostic laparoscopy, illustrating the diagnostic challenges and the need for clinician awareness of this adverse effect. A literature review accompanies the case, summarizing the epidemiology, clinical manifestations, and outcomes of this condition.
Case Description/Methods: A 41-year-old white female with a history of hypertension, asthma, gastric sleeve, and cholecystectomy presented with recurrent episodes of periumbilical and epigastric abdominal pain, nausea, vomiting, and watery diarrhea starting one week after beginning lisinopril-hydrochlorothiazide. Initially misdiagnosed with gastroenteritis, her condition worsened, leading to a diagnosis of small bowel obstruction. CT scans revealed thickened proximal jejunum and duodenum with mild ascites, and laparoscopy showed edematous small bowel without clear obstruction. The patient’s symptoms resolved within two days of discontinuing lisinopril, with no recurrence at six months follow-up.
Discussion: Visceral angioedema due to ACE inhibitors, while rare, should be considered in patients with unexplained abdominal symptoms on these medications. We conducted a literature review of 35 published case reports exhibiting 40 patients diagnosed with visceral angioedema due to ACE inhibitor therapy. The condition predominantly affects females (35/40). Symptoms consisted of abdominal pain, nausea, vomiting and/or diarrhea, and began from 12 hours to 15 years after initiation of the drug; lisinopril was the most common offending agent (28/40). Imaging usually shows bowel wall thickening and edema. Diagnosis is often delayed, leading to invasive investigations including angiography (1/40), endoscopy (8/40), paracentesis (1/40), and surgery (5/40). The primary treatment is the cessation of the offending drug, which often leads to symptom resolution within 72 hours. This case highlights the importance of recognizing ACE inhibitor-associated angioedema to avoid unnecessary surgical interventions and prevent serious complications.

Figure: CT image showing markedly thickened duodenojejunal loops of bowel.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Essam Rashad indicated no relevant financial relationships.
Soukaina El Yazal indicated no relevant financial relationships.
Essam Rashad, MBBCh1, Soukaina El Yazal, MD2. P4979 - Gastroenterologist's Recognition of Rare Adverse Drug Effect Prevents Further Harm in a Patient with Small Bowel Obstruction Due to Lisinopril: A Case Report and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
