Tuesday Poster Session
Category: Small Intestine
P4980 - Crohn’s Disease Where it Isn’t: Jejunal Lipoma-Induced Intussusception
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Naveena Luke, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Naveena Luke, MD1, Tianyu She, DO2, Divya Roy, MD3, Toyooki Sonoda, MD1, Seymour Katz, MD4
1NYU Langone Health, New York, NY; 2New York University Langone Health Long Island, Mineola, NY; 3Long Island Community Hospital - NYU Langone Health System, Mineola, NY; 4NYU Grossman School of Medicine, New Hyde Park, NY
Introduction: Small bowel intussusception is a rare occurrence in adults and typically indicates an underlying gastrointestinal (GI) pathology, which may include solid masses or chronic inflammatory conditions like Crohn's disease. We present a complex case involving a patient with a history of Crohn’s and GI bleeding, who was found to have a bleeding lipoma serving as a lead point for intussusception.
Case Description/Methods: We present the case of a 70-year-old male with a history of Crohn’s and chronic GI bleeding, necessitating blood transfusions and iron infusions. Labs showed a hemoglobin level as low as 6.8 g/dL, iron level at 18 µg/dL, iron saturation at 5%, and a ferritin level of 13 ng/dL. The patient reported dark stools (guaiac positive), abdominal pain, and fatigue, but denied any hematochezia. Initial endoscopic examinations revealed gastritis but were otherwise inconclusive. Capsule endoscopy identified a bleeding site in the proximal jejunum along with ulcerations in the jejunum and ileum, consistent with Crohn's. The patient was started on mesalamine, which effectively controlled his symptoms but did not resolve his anemia. A double-balloon enteroscopy revealed a 5-cm frond-like villous mass in the jejunum, without active inflammation. Subsequent imaging with computed tomography (CT) and magnetic resonance enterography (MRE) confirmed the presence of a jejunal lipoma, which was acting as a lead point for intussusception. The patient underwent a laparoscopic small bowel resection with jejuno-jejunal anastomosis. The surgery was well tolerated, and his hemoglobin levels have remained stable postoperatively.
Discussion: In adults, approximately 90% of intussusceptions are attributed to a pathological lead point. In Crohn's, inflammatory infiltrates can form granulomas that act as a lead point. Similarly, solid tumors, such as lipomas, can also serve as lead points. In this patient, the lipoma was initially obscured by the Crohn’s diagnosis, complicating the identification of the intussusception source and subsequent treatment. Given the rarity of symptomatic small bowel lipomas, there is no consensus on their management. However, surgical intervention is generally recommended because it is challenging to rule out malignancy, and management guidelines for colonic lipomas are often applied. This case exemplifies the importance of considering multiple underlying pathologies in patients with complex GI symptoms and highlights the need for a thorough diagnostic approach to guide effective treatment.

Disclosures:
Naveena Luke, MD1, Tianyu She, DO2, Divya Roy, MD3, Toyooki Sonoda, MD1, Seymour Katz, MD4. P4980 - Crohn’s Disease Where it Isn’t: Jejunal Lipoma-Induced Intussusception, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2New York University Langone Health Long Island, Mineola, NY; 3Long Island Community Hospital - NYU Langone Health System, Mineola, NY; 4NYU Grossman School of Medicine, New Hyde Park, NY
Introduction: Small bowel intussusception is a rare occurrence in adults and typically indicates an underlying gastrointestinal (GI) pathology, which may include solid masses or chronic inflammatory conditions like Crohn's disease. We present a complex case involving a patient with a history of Crohn’s and GI bleeding, who was found to have a bleeding lipoma serving as a lead point for intussusception.
Case Description/Methods: We present the case of a 70-year-old male with a history of Crohn’s and chronic GI bleeding, necessitating blood transfusions and iron infusions. Labs showed a hemoglobin level as low as 6.8 g/dL, iron level at 18 µg/dL, iron saturation at 5%, and a ferritin level of 13 ng/dL. The patient reported dark stools (guaiac positive), abdominal pain, and fatigue, but denied any hematochezia. Initial endoscopic examinations revealed gastritis but were otherwise inconclusive. Capsule endoscopy identified a bleeding site in the proximal jejunum along with ulcerations in the jejunum and ileum, consistent with Crohn's. The patient was started on mesalamine, which effectively controlled his symptoms but did not resolve his anemia. A double-balloon enteroscopy revealed a 5-cm frond-like villous mass in the jejunum, without active inflammation. Subsequent imaging with computed tomography (CT) and magnetic resonance enterography (MRE) confirmed the presence of a jejunal lipoma, which was acting as a lead point for intussusception. The patient underwent a laparoscopic small bowel resection with jejuno-jejunal anastomosis. The surgery was well tolerated, and his hemoglobin levels have remained stable postoperatively.
Discussion: In adults, approximately 90% of intussusceptions are attributed to a pathological lead point. In Crohn's, inflammatory infiltrates can form granulomas that act as a lead point. Similarly, solid tumors, such as lipomas, can also serve as lead points. In this patient, the lipoma was initially obscured by the Crohn’s diagnosis, complicating the identification of the intussusception source and subsequent treatment. Given the rarity of symptomatic small bowel lipomas, there is no consensus on their management. However, surgical intervention is generally recommended because it is challenging to rule out malignancy, and management guidelines for colonic lipomas are often applied. This case exemplifies the importance of considering multiple underlying pathologies in patients with complex GI symptoms and highlights the need for a thorough diagnostic approach to guide effective treatment.

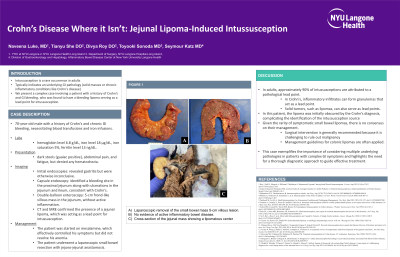
Figure: A) Laparoscopic removal of the small bowel mass 5-cm villous lesion. B) No evidence of active inflammatory bowel disease. C) Cross-section of the jejunal mass showing a lipomatous center
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Tianyu She indicated no relevant financial relationships.
Divya Roy indicated no relevant financial relationships.
Toyooki Sonoda indicated no relevant financial relationships.
Seymour Katz indicated no relevant financial relationships.
Naveena Luke, MD1, Tianyu She, DO2, Divya Roy, MD3, Toyooki Sonoda, MD1, Seymour Katz, MD4. P4980 - Crohn’s Disease Where it Isn’t: Jejunal Lipoma-Induced Intussusception, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
