Tuesday Poster Session
Category: Small Intestine
P4984 - Suboptimal Screening in Peutz-Jeghers Syndrome: A Case of Duodenal Adenocarcinoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AE
Abigail L. Ellington, MD
Atrium Health Wake Forest Baptist
Winston Salem, NC
Presenting Author(s)
Abigail L. Ellington, MD1, Alyssa A. Guo, MD1, Stephanie Brinton, MD1, Maria Krakovski, BS2, Blake Bentley, MD1, William Lippert, MD, MPH1
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Peutz-Jeghers Syndrome (PJS) is characterized by gastrointestinal (GI) hamartomatous polyps, pigmented skin lesions, and increased malignancy risk. We present a patient with suboptimal PJS screening who developed duodenal adenocarcinoma. We review the pathophysiology, symptoms, and GI cancer screening recommendations for this understudied disease.
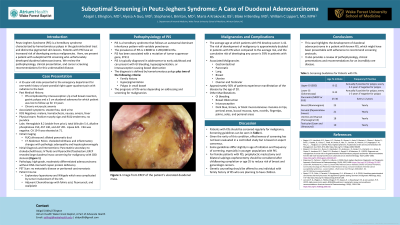
Case Description/Methods: A 35-year-old male with a 15-year history of PJS presented with acute post-prandial RUQ abdominal pain, steatorrhea, and dark urine. His only screening endoscopy was 1.5 years prior to presentation with a 5 cm duodenal adenoma and he had been otherwise been lost to follow-up. His vital signs were within normal limits. He had a positive murphy sign, RUQ tenderness, and no jaundice on exam. Initial labs showed transaminitis and an elevated CA 19-9. Imaging revealed a dilated pancreatic duct, choledocholithiasis, lymphadenopathy, and hepatosplenomegaly. ERCP found an ulcerated duodenal mass (Figure 1) with common bile duct stenosis. Biopsy demonstrated high-grade, moderately differentiated adenocarcinoma. Staging studies were negative for metastatic disease including peritoneal carcinomatosis. He then underwent a surgically complex ex-lap and Whipple operation involving the IVC, requiring vascular surgery intervention. He was discharged home with plans for further management with oncology.
Discussion: PJS has an autosomal dominant inheritance with variable penetrance and is associated with mutation of tumor suppression gene, STK11. Pigmented skin lesions and hamartomatous polyps are characteristic findings. Other symptoms include occult bleeding, bowel obstruction, and intussusception.
PJS confers nearly double the average risk of malignancy with a cumulative risk of developing any cancer of 93%. Malignancies may arise from various organs; thus, screening guidelines have been developed. For GI screening, baseline EGD and colonoscopy are recommended at age 12. If polyps are present, testing should be repeated annually. If polyps are absent, EGD should be repeated every 2-3 years and colonoscopy every 1-3 years. MRCP screening should start at age 25-30 with repeat every 1-2 years. Our patient unfortunately went 13 years without appropriate screening after his initial diagnosis. This case highlights the importance of physicians who care for PJS patients to be familiar with these guidelines and emphasize the importance of screening for malignancies to their patients.

Disclosures:
Abigail L. Ellington, MD1, Alyssa A. Guo, MD1, Stephanie Brinton, MD1, Maria Krakovski, BS2, Blake Bentley, MD1, William Lippert, MD, MPH1. P4984 - Suboptimal Screening in Peutz-Jeghers Syndrome: A Case of Duodenal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Peutz-Jeghers Syndrome (PJS) is characterized by gastrointestinal (GI) hamartomatous polyps, pigmented skin lesions, and increased malignancy risk. We present a patient with suboptimal PJS screening who developed duodenal adenocarcinoma. We review the pathophysiology, symptoms, and GI cancer screening recommendations for this understudied disease.
Case Description/Methods: A 35-year-old male with a 15-year history of PJS presented with acute post-prandial RUQ abdominal pain, steatorrhea, and dark urine. His only screening endoscopy was 1.5 years prior to presentation with a 5 cm duodenal adenoma and he had been otherwise been lost to follow-up. His vital signs were within normal limits. He had a positive murphy sign, RUQ tenderness, and no jaundice on exam. Initial labs showed transaminitis and an elevated CA 19-9. Imaging revealed a dilated pancreatic duct, choledocholithiasis, lymphadenopathy, and hepatosplenomegaly. ERCP found an ulcerated duodenal mass (Figure 1) with common bile duct stenosis. Biopsy demonstrated high-grade, moderately differentiated adenocarcinoma. Staging studies were negative for metastatic disease including peritoneal carcinomatosis. He then underwent a surgically complex ex-lap and Whipple operation involving the IVC, requiring vascular surgery intervention. He was discharged home with plans for further management with oncology.
Discussion: PJS has an autosomal dominant inheritance with variable penetrance and is associated with mutation of tumor suppression gene, STK11. Pigmented skin lesions and hamartomatous polyps are characteristic findings. Other symptoms include occult bleeding, bowel obstruction, and intussusception.
PJS confers nearly double the average risk of malignancy with a cumulative risk of developing any cancer of 93%. Malignancies may arise from various organs; thus, screening guidelines have been developed. For GI screening, baseline EGD and colonoscopy are recommended at age 12. If polyps are present, testing should be repeated annually. If polyps are absent, EGD should be repeated every 2-3 years and colonoscopy every 1-3 years. MRCP screening should start at age 25-30 with repeat every 1-2 years. Our patient unfortunately went 13 years without appropriate screening after his initial diagnosis. This case highlights the importance of physicians who care for PJS patients to be familiar with these guidelines and emphasize the importance of screening for malignancies to their patients.

Figure: Figure 1. Image from ERCP of the patient’s ulcerated duodenal mass
Disclosures:
Abigail Ellington indicated no relevant financial relationships.
Alyssa Guo indicated no relevant financial relationships.
Stephanie Brinton indicated no relevant financial relationships.
Maria Krakovski indicated no relevant financial relationships.
Blake Bentley indicated no relevant financial relationships.
William Lippert indicated no relevant financial relationships.
Abigail L. Ellington, MD1, Alyssa A. Guo, MD1, Stephanie Brinton, MD1, Maria Krakovski, BS2, Blake Bentley, MD1, William Lippert, MD, MPH1. P4984 - Suboptimal Screening in Peutz-Jeghers Syndrome: A Case of Duodenal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
