Tuesday Poster Session
Category: Small Intestine
P4989 - Duodenal Bulb Adenocarcinoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mohammad N. Kloub, MD
New York Medical College - Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Mohammad N. Kloub, MD1, Raed Atiyat, MD1, Byron Okwesili, MD1, Muhammad Hussain, MD1, Anoud Alatiyat, MD2, Atheer Anwar, MD3, Mehul Shah, MD1
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2Montclair State University, Montclair, NJ; 3Mutah University, Newark, NJ
Introduction: About 0.3% to 0.5% of gastrointestinal malignancies are duodenal adenocarcinomas, an uncommon gastrointestinal malignancy that was first described by Hamburger in 1746. Although duodenal adenocarcinomas cause the majority of small intestine adenocarcinomas, mainly in the descending duodenum (D2), they are extremely uncommon in the duodenal bulb [1,2]. We present a patient who came in with symptomatic anemia from gastrointestinal blood loss due to adenocarcinoma of the duodenum bulb.
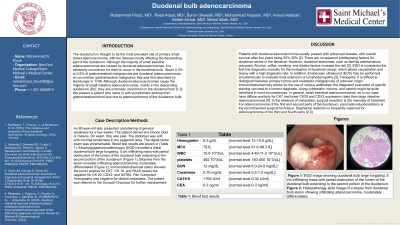
Case Description/Methods: An 80-year-old lady presented complaining of general weakness for a few weeks. The patient denied any bloody stool or melena. On exam, She was pale. The abdomen was soft, with minimal tenderness in the epigastric area. The digital rectal exam was unremarkable. Blood test results are shown in (Table 1). Esophagogastroduodenoscopy (EGD) revealed a distal duodenal bulb large fungating, 5 cm infiltrating mass with partial obstruction of the lumen of the duodenal bulb extending to the second portion of the duodenum (Figure 1). Biopsies from the lesion revealed infiltrating adenocarcinoma, moderately differentiated (Figure 2). Immunohistochemical stains showed the tumor positive for CK7, CK 19, and PAX8 (weak) but negative for CK 20, CDX2, and SATB2. Pan Computed Tomography was negative for distant metastasis. The patient was referred to the Surgical-Oncology for further management.
Discussion: Patients with duodenal adenocarcinoma usually present with advanced disease, with overall survival after five years being 25%-35%. There are no apparent predisposing factors for duodenal cancer in the literature. However, duodenal adenomas, such as familial adenomatous polyposis, Alcohol, coffee, smoking, and dietary factors increase the risk. EGD is considered the first-line diagnostic modality for the evaluation of duodenal cancer, which allows visualization and biopsy with a high diagnostic rate. In addition, Endoscopic ultrasound (EUS) may be performed simultaneously to evaluate local extension or lymphadenopathy. Frequently, It is difficult to distinguish between primary tumors and metastatic malignancies of unknown origin. Immunohistochemistry with specific staining can lead to a correct diagnosis. In the absence of metastasis, surgical resection is the mainstay of treatment. For adenocarcinoma of the first and second parts of the duodenum, pancreaticoduodenectomy is the recommended surgical technique. Segmental resection is frequently reserved for adenocarcinoma of the third and fourth parts.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mohammad N. Kloub, MD1, Raed Atiyat, MD1, Byron Okwesili, MD1, Muhammad Hussain, MD1, Anoud Alatiyat, MD2, Atheer Anwar, MD3, Mehul Shah, MD1. P4989 - Duodenal Bulb Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2Montclair State University, Montclair, NJ; 3Mutah University, Newark, NJ
Introduction: About 0.3% to 0.5% of gastrointestinal malignancies are duodenal adenocarcinomas, an uncommon gastrointestinal malignancy that was first described by Hamburger in 1746. Although duodenal adenocarcinomas cause the majority of small intestine adenocarcinomas, mainly in the descending duodenum (D2), they are extremely uncommon in the duodenal bulb [1,2]. We present a patient who came in with symptomatic anemia from gastrointestinal blood loss due to adenocarcinoma of the duodenum bulb.
Case Description/Methods: An 80-year-old lady presented complaining of general weakness for a few weeks. The patient denied any bloody stool or melena. On exam, She was pale. The abdomen was soft, with minimal tenderness in the epigastric area. The digital rectal exam was unremarkable. Blood test results are shown in (Table 1). Esophagogastroduodenoscopy (EGD) revealed a distal duodenal bulb large fungating, 5 cm infiltrating mass with partial obstruction of the lumen of the duodenal bulb extending to the second portion of the duodenum (Figure 1). Biopsies from the lesion revealed infiltrating adenocarcinoma, moderately differentiated (Figure 2). Immunohistochemical stains showed the tumor positive for CK7, CK 19, and PAX8 (weak) but negative for CK 20, CDX2, and SATB2. Pan Computed Tomography was negative for distant metastasis. The patient was referred to the Surgical-Oncology for further management.
Discussion: Patients with duodenal adenocarcinoma usually present with advanced disease, with overall survival after five years being 25%-35%. There are no apparent predisposing factors for duodenal cancer in the literature. However, duodenal adenomas, such as familial adenomatous polyposis, Alcohol, coffee, smoking, and dietary factors increase the risk. EGD is considered the first-line diagnostic modality for the evaluation of duodenal cancer, which allows visualization and biopsy with a high diagnostic rate. In addition, Endoscopic ultrasound (EUS) may be performed simultaneously to evaluate local extension or lymphadenopathy. Frequently, It is difficult to distinguish between primary tumors and metastatic malignancies of unknown origin. Immunohistochemistry with specific staining can lead to a correct diagnosis. In the absence of metastasis, surgical resection is the mainstay of treatment. For adenocarcinoma of the first and second parts of the duodenum, pancreaticoduodenectomy is the recommended surgical technique. Segmental resection is frequently reserved for adenocarcinoma of the third and fourth parts.

Figure:
Figure 1
EGD image showing duodenal bulb large fungating, 5 cm infiltrating mass with partial obstruction of the lumen of the duodenal bulb extending to the second portion of the duodenum.
Figure 2
Histopathology slide image of a biopsy from duodenal bulb lesion showing infiltrating adenocarcinoma, moderately differentiated.
Figure 1
EGD image showing duodenal bulb large fungating, 5 cm infiltrating mass with partial obstruction of the lumen of the duodenal bulb extending to the second portion of the duodenum.
Figure 2
Histopathology slide image of a biopsy from duodenal bulb lesion showing infiltrating adenocarcinoma, moderately differentiated.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mohammad Kloub indicated no relevant financial relationships.
Raed Atiyat indicated no relevant financial relationships.
Byron Okwesili indicated no relevant financial relationships.
Muhammad Hussain indicated no relevant financial relationships.
Anoud Alatiyat indicated no relevant financial relationships.
Atheer Anwar indicated no relevant financial relationships.
Mehul Shah indicated no relevant financial relationships.
Mohammad N. Kloub, MD1, Raed Atiyat, MD1, Byron Okwesili, MD1, Muhammad Hussain, MD1, Anoud Alatiyat, MD2, Atheer Anwar, MD3, Mehul Shah, MD1. P4989 - Duodenal Bulb Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
