Tuesday Poster Session
Category: Small Intestine
P4995 - Successful Multidisciplinary Treatment of Small Bowel Obstruction with Ileal Stricture Resulting in Bowel Perforation in the Setting of Multidrug-Resistant Gastrointestinal Tuberculosis: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Michael Ladna, MD
University of California Davis Health Graduate Medical Education
Sacramento, CA
Presenting Author(s)
Michael Ladna, MD
University of California Davis Health Graduate Medical Education, Sacramento, CA
Introduction: We present the case of a patient with MDR GI TB complicated by strictures of the ileum and jejunum, small bowel obstruction, and perforation successfully treated with bowel rest, TPN, IV antibiotics, and right hemicolectomy with creation of ileal-colon anastomosis.
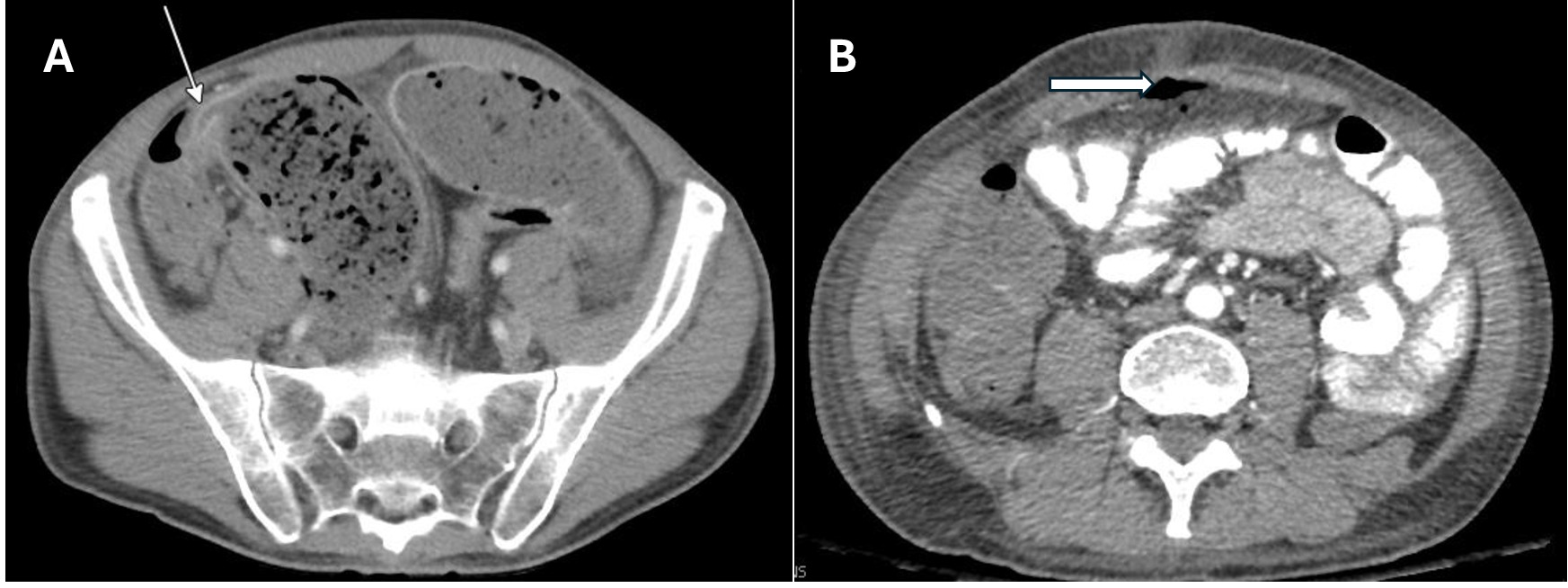
Case Description/Methods: A male in his 40s on BPAL-M regimen for MDR pulmonary TB presented to ED with abdominal pain, vomiting, and cessation of bowel movements. CT abdomen/pelvis showed small bowel obstruction with a terminal ileal stricture and focal jejunal narrowing consistent with a second stricture consistent with GI TB. Acute care surgery recommended bowel rest and decompression however declined NG tube. A PICC line was placed and he was started on TPN for nutrition. His oral anti-TB regimen was held and he was started on IV linezolid, IV moxifloxacin, IV meropenem, and IV ampicillin-sulbactam. Stress dose corticosteroids were added alongside IV Bactrim for PJP prophylaxis. On day 18 of hospitalization he developed severe abdominal pain and CT abdomen/pelvis showed pneumoperitoneum consistent with bowel perforation. He was taken emergently to the OR for exploratory laparotomy. A perforation was found in the terminal ileum and a right hemicolectomy was done. On post-op day 2, he returned to the OR for stapling of the ileocolic anastomosis and fascial closure. He tolerated the initiation of diet and resumption of oral anti-TB regimen and was discharged home after a 23-day hospitalization.
Discussion: GI TB can be challenging to diagnose, in part due to non-specific symptoms that mimic other pathologies but also in that it could present without pulmonary involvement. GI TB can be especially challenging to cure due to impairment in the absorption of oral anti-tuberculosis medications. MDR-TB further complicates the therapeutic plan and is associated with higher mortality compared to drug-susceptible TB. Most of the agents in the BPAL-M regimen are not available in IV formulation. High-dose corticosteroids decrease the risk of strictures and obstruction, Complications of GI TB include strictures (most commonly in the ileocecal area of the small bowel), bowel obstruction, and perforation. These patients are poor surgical candidates due to often being severely malnourished and as such ensuring timely diagnosis and initiation of therapy is crucial to prevent progression to these severe complications. If emergent surgery is required such as in our case, resection anastomosis is preferred over primary closure due to better outcomes.
Disclosures:
Michael Ladna, MD. P4995 - Successful Multidisciplinary Treatment of Small Bowel Obstruction with Ileal Stricture Resulting in Bowel Perforation in the Setting of Multidrug-Resistant Gastrointestinal Tuberculosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of California Davis Health Graduate Medical Education, Sacramento, CA
Introduction: We present the case of a patient with MDR GI TB complicated by strictures of the ileum and jejunum, small bowel obstruction, and perforation successfully treated with bowel rest, TPN, IV antibiotics, and right hemicolectomy with creation of ileal-colon anastomosis.
Case Description/Methods: A male in his 40s on BPAL-M regimen for MDR pulmonary TB presented to ED with abdominal pain, vomiting, and cessation of bowel movements. CT abdomen/pelvis showed small bowel obstruction with a terminal ileal stricture and focal jejunal narrowing consistent with a second stricture consistent with GI TB. Acute care surgery recommended bowel rest and decompression however declined NG tube. A PICC line was placed and he was started on TPN for nutrition. His oral anti-TB regimen was held and he was started on IV linezolid, IV moxifloxacin, IV meropenem, and IV ampicillin-sulbactam. Stress dose corticosteroids were added alongside IV Bactrim for PJP prophylaxis. On day 18 of hospitalization he developed severe abdominal pain and CT abdomen/pelvis showed pneumoperitoneum consistent with bowel perforation. He was taken emergently to the OR for exploratory laparotomy. A perforation was found in the terminal ileum and a right hemicolectomy was done. On post-op day 2, he returned to the OR for stapling of the ileocolic anastomosis and fascial closure. He tolerated the initiation of diet and resumption of oral anti-TB regimen and was discharged home after a 23-day hospitalization.
Discussion: GI TB can be challenging to diagnose, in part due to non-specific symptoms that mimic other pathologies but also in that it could present without pulmonary involvement. GI TB can be especially challenging to cure due to impairment in the absorption of oral anti-tuberculosis medications. MDR-TB further complicates the therapeutic plan and is associated with higher mortality compared to drug-susceptible TB. Most of the agents in the BPAL-M regimen are not available in IV formulation. High-dose corticosteroids decrease the risk of strictures and obstruction, Complications of GI TB include strictures (most commonly in the ileocecal area of the small bowel), bowel obstruction, and perforation. These patients are poor surgical candidates due to often being severely malnourished and as such ensuring timely diagnosis and initiation of therapy is crucial to prevent progression to these severe complications. If emergent surgery is required such as in our case, resection anastomosis is preferred over primary closure due to better outcomes.
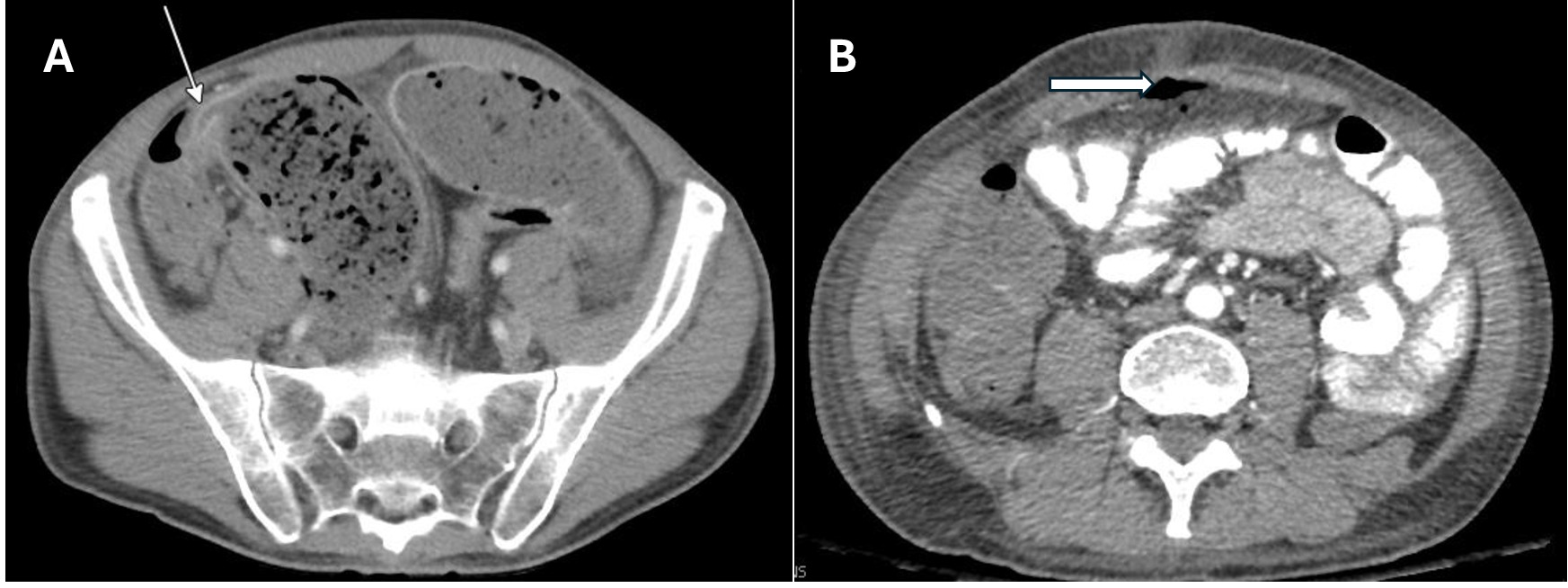
Figure: (A) Small bowel obstruction from terminal ileal stricture near the ileocecal junction (white arrow), (B) pneumoperitoneum consistent with bowel perforation (white area pointing to free air in the abdomen)
Disclosures:
Michael Ladna indicated no relevant financial relationships.
Michael Ladna, MD. P4995 - Successful Multidisciplinary Treatment of Small Bowel Obstruction with Ileal Stricture Resulting in Bowel Perforation in the Setting of Multidrug-Resistant Gastrointestinal Tuberculosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
