Tuesday Poster Session
Category: Small Intestine
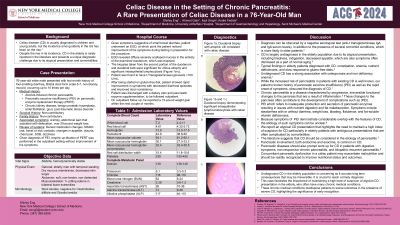
P4996 - Celiac Disease in the Setting of Chronic Pancreatitis: A Rare Presentation of Celiac Disease in a 76-Year-Old Man
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SE
Shirley Eng
New York Medical College
New York, NY
Presenting Author(s)
Shirley Eng, 1, Ahmed Gabr, 1, Ikjot Singh, MD2, Andre Fedida, MD3
1New York Medical College, New York, NY; 2University at Buffalo, Buffalo, NY; 3Allied Digestive Health, Newark, NJ
Introduction: While Celiac disease is usually diagnosed in children and young adults, the incidence of celiac disease among elderly individuals in the United States has been on the rise. Despite this steady rise in incidence, celiac disease in the elderly has been rarely reported in the literature and presents diagnostic challenges due to atypical presentations and comorbidities.
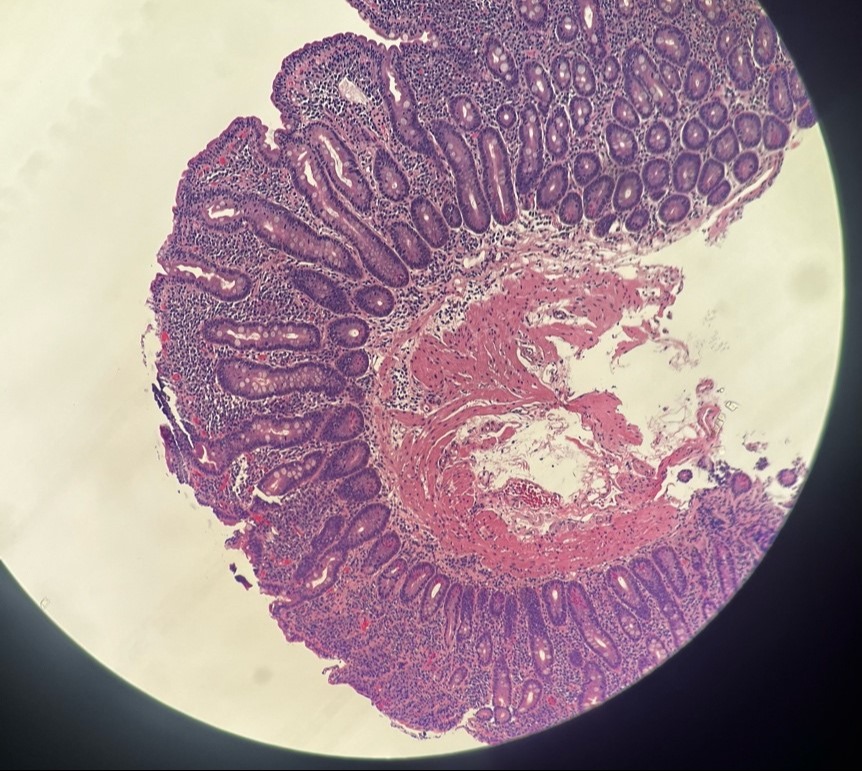
Case Description/Methods: We report a case of a 76-year-old male with past medical history of alcohol-induced chronic pancreatitis with pancreatic exocrine insufficiency (PEI) on pancreatic enzyme replacement therapy (PERT) presenting with a two-month history of foul smelling, non-bloody, and mucoid diarrhea, occurring up to 10 times per day. While fasting in preparation for Esophagogastroduodenoscopy (EGD), the patient noticed improvement of his symptoms. EGD biopsies taken from the duodenum were significant for villous atrophy and significant intraepithelial lymphocytosis. Additionally, the patient was found to have elevated t-Transglutaminase IgA levels. Celiac disease was diagnosed, and patient was started on a gluten free diet and showed rapid improvement in symptoms with decreased diarrheal episodes and improved stool consistency.
Discussion: This case underscores the importance of considering celiac disease in elderly patients with ambiguous symptoms, particularly when complicated by other chronic illnesses. Prompt recognition and adherence to a gluten-free diet are crucial to mitigate the long-term consequences of undiagnosed celiac disease in this vulnerable population.
We report an atypical celiac disease presentation that highlights the need to maintain a high index of suspicion for celiac disease particularly in elderly patients with ambiguous presentations that are often complicated by comorbidities. The literature suggests that celiac disease should be considered in the etiology of pancreatitis. Pancreatic involvement, both endocrine and exocrine, is common in celiac disease. Conversely, pancreatic diseases should also prompt work up for celiac disease in patients with digestive symptoms, non-responsive chronic pancreatitis, and idiopathic recurrent pancreatitis. Concomitant pancreatic dysfunction in a celiac patient may exacerbate malnutrition and should be readily recognized in order to improve nutritional status and outcomes.
Disclosures:
Shirley Eng, 1, Ahmed Gabr, 1, Ikjot Singh, MD2, Andre Fedida, MD3. P4996 - Celiac Disease in the Setting of Chronic Pancreatitis: A Rare Presentation of Celiac Disease in a 76-Year-Old Man, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York Medical College, New York, NY; 2University at Buffalo, Buffalo, NY; 3Allied Digestive Health, Newark, NJ
Introduction: While Celiac disease is usually diagnosed in children and young adults, the incidence of celiac disease among elderly individuals in the United States has been on the rise. Despite this steady rise in incidence, celiac disease in the elderly has been rarely reported in the literature and presents diagnostic challenges due to atypical presentations and comorbidities.
Case Description/Methods: We report a case of a 76-year-old male with past medical history of alcohol-induced chronic pancreatitis with pancreatic exocrine insufficiency (PEI) on pancreatic enzyme replacement therapy (PERT) presenting with a two-month history of foul smelling, non-bloody, and mucoid diarrhea, occurring up to 10 times per day. While fasting in preparation for Esophagogastroduodenoscopy (EGD), the patient noticed improvement of his symptoms. EGD biopsies taken from the duodenum were significant for villous atrophy and significant intraepithelial lymphocytosis. Additionally, the patient was found to have elevated t-Transglutaminase IgA levels. Celiac disease was diagnosed, and patient was started on a gluten free diet and showed rapid improvement in symptoms with decreased diarrheal episodes and improved stool consistency.
Discussion: This case underscores the importance of considering celiac disease in elderly patients with ambiguous symptoms, particularly when complicated by other chronic illnesses. Prompt recognition and adherence to a gluten-free diet are crucial to mitigate the long-term consequences of undiagnosed celiac disease in this vulnerable population.
We report an atypical celiac disease presentation that highlights the need to maintain a high index of suspicion for celiac disease particularly in elderly patients with ambiguous presentations that are often complicated by comorbidities. The literature suggests that celiac disease should be considered in the etiology of pancreatitis. Pancreatic involvement, both endocrine and exocrine, is common in celiac disease. Conversely, pancreatic diseases should also prompt work up for celiac disease in patients with digestive symptoms, non-responsive chronic pancreatitis, and idiopathic recurrent pancreatitis. Concomitant pancreatic dysfunction in a celiac patient may exacerbate malnutrition and should be readily recognized in order to improve nutritional status and outcomes.
Figure: Duodenal mucosa with atrophic villi consistent with celiac disease.
Disclosures:
Shirley Eng indicated no relevant financial relationships.
Ahmed Gabr indicated no relevant financial relationships.
Ikjot Singh indicated no relevant financial relationships.
Andre Fedida indicated no relevant financial relationships.
Shirley Eng, 1, Ahmed Gabr, 1, Ikjot Singh, MD2, Andre Fedida, MD3. P4996 - Celiac Disease in the Setting of Chronic Pancreatitis: A Rare Presentation of Celiac Disease in a 76-Year-Old Man, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

