Tuesday Poster Session
Category: Small Intestine
P5004 - Cystic Fibrosis and Recurrent Distal Intestinal Obstruction Syndrome
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Arvin Jeremy Tan, MD
University of Hawaii, John A. Burns School of Medicine
Honolulu, HI
Presenting Author(s)
Arvin Jeremy Tan, MD1, Toru Nakata, MD, PhD1, Shanelle Katrina Tan, BS2, Traci T. Murakami, MD, FACG3
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2University of Santo Tomas, Manila, National Capital Region, Philippines; 3The Queen's Medical Center, Honolulu, HI
Introduction: Distal intestinal obstruction syndrome (DIOS) is unique to Cystic Fibrosis (CF). It is characterized by an acute complete or incomplete obstruction of the ileocecum by inspissated intestinal contents. It occurs in 10% to 47% of patients with CF, with a recurrence rate as high as 77%. Here, we report a case of a patient with cystic fibrosis presenting with incomplete DIOS.
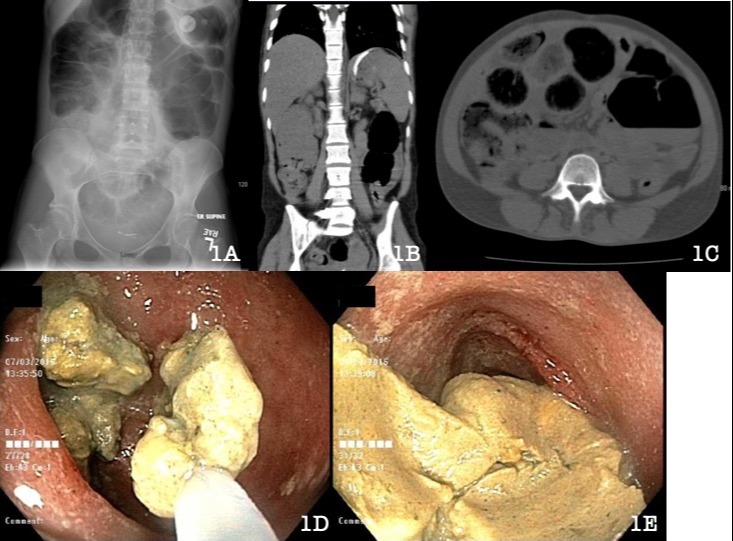
Case Description/Methods: A 26-year-old female with a history of cystic fibrosis, meconium ileus, post-bilateral lung transplant, diabetes, chronic pancreatitis with pancreatic insufficiency, and prior DIOS presented to the ED with severe peri-umbilical pain, nausea, and abdominal distention. She was given rectal lactulose, mineral oil enema, and mucomyst and was discharged after resolution of symptoms. The following day, however, she had a recurrence of abdominal pain and distention. Radiograph revealed colonic distension (Image 1A), and she was hospitalized due to concerns for ileus vs. distal bowel obstruction. CT showed DIOS (Image 1B-1C), and barium enema showed contrast uptake through the cecum but not the terminal ileum. She developed increasing intra-abdominal pressures, which led to acute hypercapnic and hypoxemic respiratory failure. She was subsequently taken to the ICU, where she was intubated and mechanically ventilated. Urgent colonoscopy revealed a large amount of semi-solid stool in the terminal ileum which was removed with a roth net, snare, and sterile water lavage (Image 1D-1E). This resulted in disimpaction and significant clinical improvement. She was maintained on a regimen of Miralax, Senna, Lactulose, and enemas. The patient was then transferred to an outside hospital for higher level of care given her post-transplant status. There, she developed ARDS requiring ECMO with de-cannulation and clinical improvement after 2 months.
Discussion: Patients with CF are prone to intestinal obstruction starting in early life due to the alteration of gut physiology. It commonly presents with abdominal pain and is associated with meconium ileus, liver disease, diabetes, Pseudomonas colonization, and pancreatic insufficiency. Our patient presented with the listed risk factors except for liver disease. Treatment involves clearance of luminal contents with laxatives and mucolytic agents. Surgical decompression is reserved for refractory cases due to high morbidity. Prevention of complete obstruction is important; hence, providers should have a high index of suspicion for patients with CF and abdominal pain.
Disclosures:
Arvin Jeremy Tan, MD1, Toru Nakata, MD, PhD1, Shanelle Katrina Tan, BS2, Traci T. Murakami, MD, FACG3. P5004 - Cystic Fibrosis and Recurrent Distal Intestinal Obstruction Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2University of Santo Tomas, Manila, National Capital Region, Philippines; 3The Queen's Medical Center, Honolulu, HI
Introduction: Distal intestinal obstruction syndrome (DIOS) is unique to Cystic Fibrosis (CF). It is characterized by an acute complete or incomplete obstruction of the ileocecum by inspissated intestinal contents. It occurs in 10% to 47% of patients with CF, with a recurrence rate as high as 77%. Here, we report a case of a patient with cystic fibrosis presenting with incomplete DIOS.
Case Description/Methods: A 26-year-old female with a history of cystic fibrosis, meconium ileus, post-bilateral lung transplant, diabetes, chronic pancreatitis with pancreatic insufficiency, and prior DIOS presented to the ED with severe peri-umbilical pain, nausea, and abdominal distention. She was given rectal lactulose, mineral oil enema, and mucomyst and was discharged after resolution of symptoms. The following day, however, she had a recurrence of abdominal pain and distention. Radiograph revealed colonic distension (Image 1A), and she was hospitalized due to concerns for ileus vs. distal bowel obstruction. CT showed DIOS (Image 1B-1C), and barium enema showed contrast uptake through the cecum but not the terminal ileum. She developed increasing intra-abdominal pressures, which led to acute hypercapnic and hypoxemic respiratory failure. She was subsequently taken to the ICU, where she was intubated and mechanically ventilated. Urgent colonoscopy revealed a large amount of semi-solid stool in the terminal ileum which was removed with a roth net, snare, and sterile water lavage (Image 1D-1E). This resulted in disimpaction and significant clinical improvement. She was maintained on a regimen of Miralax, Senna, Lactulose, and enemas. The patient was then transferred to an outside hospital for higher level of care given her post-transplant status. There, she developed ARDS requiring ECMO with de-cannulation and clinical improvement after 2 months.
Discussion: Patients with CF are prone to intestinal obstruction starting in early life due to the alteration of gut physiology. It commonly presents with abdominal pain and is associated with meconium ileus, liver disease, diabetes, Pseudomonas colonization, and pancreatic insufficiency. Our patient presented with the listed risk factors except for liver disease. Treatment involves clearance of luminal contents with laxatives and mucolytic agents. Surgical decompression is reserved for refractory cases due to high morbidity. Prevention of complete obstruction is important; hence, providers should have a high index of suspicion for patients with CF and abdominal pain.
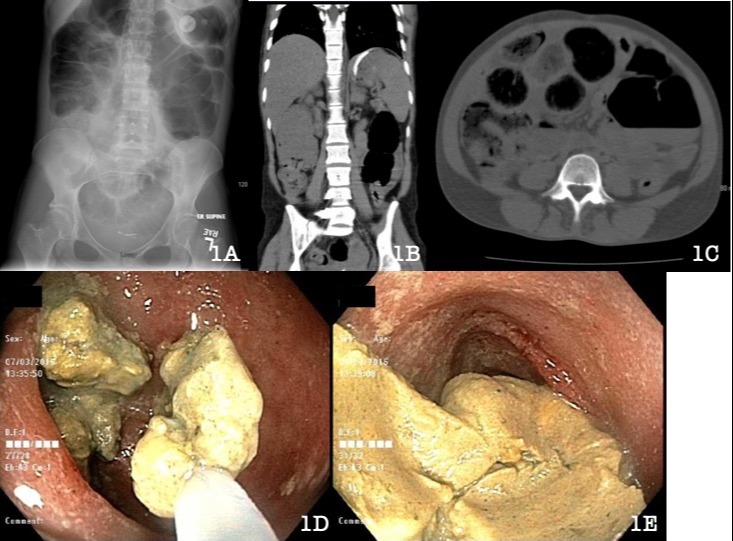
Figure: 1A: Radiograph of the abdomen showing mild colonic distention and less pronounced small bowel distention.
1B-1C: CT imaging of the abdomen and pelvis showing abnormal dilated loops of small bowel containing fecal material and mild wall thickening consistent with DIOS
ID-1E: Colonoscopy images showing impacted stool and retrieval/ disimpaction with a roth snare.
1B-1C: CT imaging of the abdomen and pelvis showing abnormal dilated loops of small bowel containing fecal material and mild wall thickening consistent with DIOS
ID-1E: Colonoscopy images showing impacted stool and retrieval/ disimpaction with a roth snare.
Disclosures:
Arvin Jeremy Tan indicated no relevant financial relationships.
Toru Nakata indicated no relevant financial relationships.
Shanelle Katrina Tan indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Arvin Jeremy Tan, MD1, Toru Nakata, MD, PhD1, Shanelle Katrina Tan, BS2, Traci T. Murakami, MD, FACG3. P5004 - Cystic Fibrosis and Recurrent Distal Intestinal Obstruction Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
