Tuesday Poster Session
Category: Small Intestine
P5007 - A Spontaneous Submucosal Duodenal Hemorrhage in a Hemophilic Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Mustafa Saed, MS
Texas A&M School of Medicine
Dallas, TX
Presenting Author(s)
Racha Cherradi, BS1, Mustafa Saed, MS1, Naser Asfoor, DO2, Omair Atiq, MD3
1Texas A&M School of Medicine, Dallas, TX; 2Texas College of Osteopathic Medicine, Fort Worth, TX; 3Texas Health Digestive Specialists, Fort Worth, TX
Introduction:
Gastrointestinal bleeding poses a common challenge in hospitals, linked to higher mortality rates and various complications. Mutations in Factor VIII/IX play a significant role in bleeding tendencies and clinical manifestations in those with these conditions. Vomiting material resembling coffee grounds or red blood, known as hematemesis, often indicates bleeding near the ligament of Treitz. We herein report an atypical case of a 32-year-old patient with poorly managed hemophilia A, who experienced multiple episodes of sudden hematemesis and imaging findings consistent with duodenal wall thickening. This led to the diagnosis of submucosal duodenal hemorrhage.
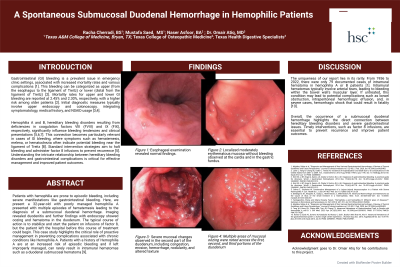
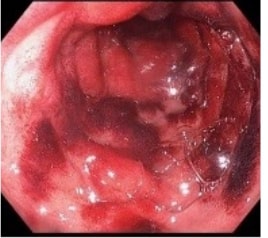
Case Description/Methods: A 32-year-old male with Hemophilia A, presented with bright red hematemesis, upper abdominal pain, and chills. A CT scan showed diffuse wall thickening in the small bowel around the duodenum. An upper GI endoscopy revealed localized moderately erythematous mucosa in the cardia and gastric fundus without any signs of bleeding. Normal findings of the esophagus were observed. Diffuse severe mucosal changes characterized by congestion, erosion, hemorrhagic appearance, nodularity, and altered texture were evident through the first three sections of the duodenum. Multiple areas with mucosal oozing were also noted. Cold forceps biopsies combined with patient’s history suggest a submucosal hemorrhage. Given the spontaneity and lack of other risk factors, this is indicative of coagulopathy, specifically factor 8 deficiency. To address the bleeding, successful hemostasis was achieved through endoscopic argon plasma coagulation.
Discussion: GI bleeding can be classified as either upper (from the esophagus to the ligament of Treitz) or lower (distal from the ligament of Treitz). The mortality rates for upper and lower GI bleeding are 2.45% and 2.30%, respectively, with an increased fatality rate in older patients. When GI bleeding is suspected, the healthcare team initiates an initial upper endoscopy and colonoscopy. Diagnosis integrates symptomatology, medical history, physical examinations, and a heavy emphasis on ongoing medications.
The uniqueness of our report lies in its rarity. From 1956 to 2022, there were 79 documented cases of intramural hematoma in hemophilia patients. Intramural hematomas typically involve arterial tears, causing bleeding within the bowel wall's muscle layer. If untreated, this condition may advance, leading to potential complications such as bowel obstruction, effusion, and hemorrhagic shock.
Disclosures:
Racha Cherradi, BS1, Mustafa Saed, MS1, Naser Asfoor, DO2, Omair Atiq, MD3. P5007 - A Spontaneous Submucosal Duodenal Hemorrhage in a Hemophilic Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas A&M School of Medicine, Dallas, TX; 2Texas College of Osteopathic Medicine, Fort Worth, TX; 3Texas Health Digestive Specialists, Fort Worth, TX
Introduction:
Gastrointestinal bleeding poses a common challenge in hospitals, linked to higher mortality rates and various complications. Mutations in Factor VIII/IX play a significant role in bleeding tendencies and clinical manifestations in those with these conditions. Vomiting material resembling coffee grounds or red blood, known as hematemesis, often indicates bleeding near the ligament of Treitz. We herein report an atypical case of a 32-year-old patient with poorly managed hemophilia A, who experienced multiple episodes of sudden hematemesis and imaging findings consistent with duodenal wall thickening. This led to the diagnosis of submucosal duodenal hemorrhage.
Case Description/Methods: A 32-year-old male with Hemophilia A, presented with bright red hematemesis, upper abdominal pain, and chills. A CT scan showed diffuse wall thickening in the small bowel around the duodenum. An upper GI endoscopy revealed localized moderately erythematous mucosa in the cardia and gastric fundus without any signs of bleeding. Normal findings of the esophagus were observed. Diffuse severe mucosal changes characterized by congestion, erosion, hemorrhagic appearance, nodularity, and altered texture were evident through the first three sections of the duodenum. Multiple areas with mucosal oozing were also noted. Cold forceps biopsies combined with patient’s history suggest a submucosal hemorrhage. Given the spontaneity and lack of other risk factors, this is indicative of coagulopathy, specifically factor 8 deficiency. To address the bleeding, successful hemostasis was achieved through endoscopic argon plasma coagulation.
Discussion: GI bleeding can be classified as either upper (from the esophagus to the ligament of Treitz) or lower (distal from the ligament of Treitz). The mortality rates for upper and lower GI bleeding are 2.45% and 2.30%, respectively, with an increased fatality rate in older patients. When GI bleeding is suspected, the healthcare team initiates an initial upper endoscopy and colonoscopy. Diagnosis integrates symptomatology, medical history, physical examinations, and a heavy emphasis on ongoing medications.
The uniqueness of our report lies in its rarity. From 1956 to 2022, there were 79 documented cases of intramural hematoma in hemophilia patients. Intramural hematomas typically involve arterial tears, causing bleeding within the bowel wall's muscle layer. If untreated, this condition may advance, leading to potential complications such as bowel obstruction, effusion, and hemorrhagic shock.
Figure: Severe mucosal changes observed in the second part of the duodenum, including congestion, erosion, hemorrhage, nodularity, and altered texture
Disclosures:
Racha Cherradi indicated no relevant financial relationships.
Mustafa Saed indicated no relevant financial relationships.
Naser Asfoor indicated no relevant financial relationships.
Omair Atiq indicated no relevant financial relationships.
Racha Cherradi, BS1, Mustafa Saed, MS1, Naser Asfoor, DO2, Omair Atiq, MD3. P5007 - A Spontaneous Submucosal Duodenal Hemorrhage in a Hemophilic Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
