Tuesday Poster Session
Category: Small Intestine
P5028 - Clearing the Air: Non-Surgical Management of Pneumatosis in Scleroderma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Jeevin S. Sandhu, DO, BA
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
Matthew Still, DO, BS1, Jeevin S. Sandhu, DO, BA2, Bianca W. Chang, MD3, Ali Rezaie, MD4
1University of Cincinnati Medical Center, Cincinnati, OH; 2Methodist Dallas Medical Center, Dallas, TX; 3Cedars-Sinai Medical Center, Los Angeles, CA; 4Cedars-Sinai Medical Center, West Hollywood, CA
Introduction: Systemic sclerosis (SSc) is a rare connective tissue disorder categorized by various systemic manifestations and organ involvement, contributing to increased morbidity and mortality. The pathogenesis involves microvascular disease and extracellular matrix deposition, affecting the skin, gastrointestinal tract, lungs, kidneys, and skeletal muscle. A rare gastrointestinal complication is pneumatosis cystoides intestinalis (PCI), characterized by intramural gas accumulation within thin-walled cysts. These bubble-like lesions, usually located in the submucosa and/or subserosa, can be accompanied by free air in the peritoneal cavity. PCI can be asymptomatic, occasionally being incidentally discovered on imaging, but can also cause abdominal pain and stool changes. These non-specific symptoms and radiographic findings can imitate genuine gastrointestinal perforations, making accurate diagnosis critical.
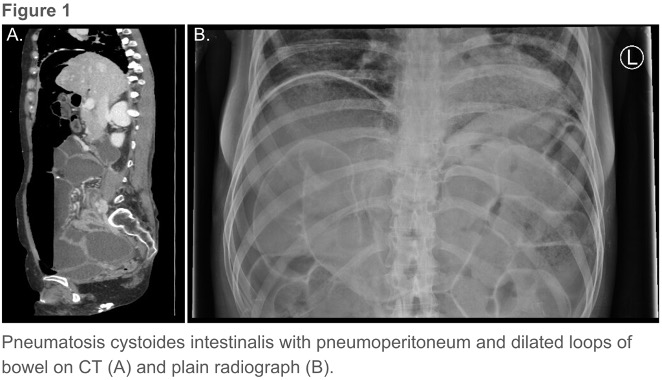
Case Description/Methods: A 27-year-old female presented with progressive dyspnea and abdominal distension for over a week. Her medical history was significant for scleroderma associated with pulmonary fibrosis, pneumothorax, calcinosis, severe lower gastrointestinal dysmotility, small intestinal bacterial overgrowth (SIBO), and recurrent small bowel obstruction (SBO). Initial examination showed severe malnutrition with an unremarkable abdominal exam. Abdominal imaging showed evidence of small bowel perforation and a large pneumoperitoneum, with dilated loops of bowel without obvious obstruction and PCI. Both gastroenterology and surgery teams agreed that an underlying pseudo-obstruction was highly probable. She was treated conservatively with broad-spectrum antibiotics, monitored closely with serial abdominal examinations, and started on total parenteral nutrition (TPN). Her dyspnea and pneumoperitoneum gradually improved. On day 15, she was discharged home on TPN after repeated imaging no longer demonstrated free air.
Discussion: Pneumatosis cystoides intestinalis is a generally benign complication of SSc and can be confused with other serious etiologies of pneumoperitoneum. Careful history-taking, examination, and imaging are imperative to avoid unnecessary surgery. Conservative management of scleroderma-associated-PCI has been documented and is appropriate and associated with better outcomes than cases where patients underwent surgical intervention. This is especially pertinent in cases without peritoneal signs, such as the case described above.
Disclosures:
Matthew Still, DO, BS1, Jeevin S. Sandhu, DO, BA2, Bianca W. Chang, MD3, Ali Rezaie, MD4. P5028 - Clearing the Air: Non-Surgical Management of Pneumatosis in Scleroderma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Cincinnati Medical Center, Cincinnati, OH; 2Methodist Dallas Medical Center, Dallas, TX; 3Cedars-Sinai Medical Center, Los Angeles, CA; 4Cedars-Sinai Medical Center, West Hollywood, CA
Introduction: Systemic sclerosis (SSc) is a rare connective tissue disorder categorized by various systemic manifestations and organ involvement, contributing to increased morbidity and mortality. The pathogenesis involves microvascular disease and extracellular matrix deposition, affecting the skin, gastrointestinal tract, lungs, kidneys, and skeletal muscle. A rare gastrointestinal complication is pneumatosis cystoides intestinalis (PCI), characterized by intramural gas accumulation within thin-walled cysts. These bubble-like lesions, usually located in the submucosa and/or subserosa, can be accompanied by free air in the peritoneal cavity. PCI can be asymptomatic, occasionally being incidentally discovered on imaging, but can also cause abdominal pain and stool changes. These non-specific symptoms and radiographic findings can imitate genuine gastrointestinal perforations, making accurate diagnosis critical.
Case Description/Methods: A 27-year-old female presented with progressive dyspnea and abdominal distension for over a week. Her medical history was significant for scleroderma associated with pulmonary fibrosis, pneumothorax, calcinosis, severe lower gastrointestinal dysmotility, small intestinal bacterial overgrowth (SIBO), and recurrent small bowel obstruction (SBO). Initial examination showed severe malnutrition with an unremarkable abdominal exam. Abdominal imaging showed evidence of small bowel perforation and a large pneumoperitoneum, with dilated loops of bowel without obvious obstruction and PCI. Both gastroenterology and surgery teams agreed that an underlying pseudo-obstruction was highly probable. She was treated conservatively with broad-spectrum antibiotics, monitored closely with serial abdominal examinations, and started on total parenteral nutrition (TPN). Her dyspnea and pneumoperitoneum gradually improved. On day 15, she was discharged home on TPN after repeated imaging no longer demonstrated free air.
Discussion: Pneumatosis cystoides intestinalis is a generally benign complication of SSc and can be confused with other serious etiologies of pneumoperitoneum. Careful history-taking, examination, and imaging are imperative to avoid unnecessary surgery. Conservative management of scleroderma-associated-PCI has been documented and is appropriate and associated with better outcomes than cases where patients underwent surgical intervention. This is especially pertinent in cases without peritoneal signs, such as the case described above.
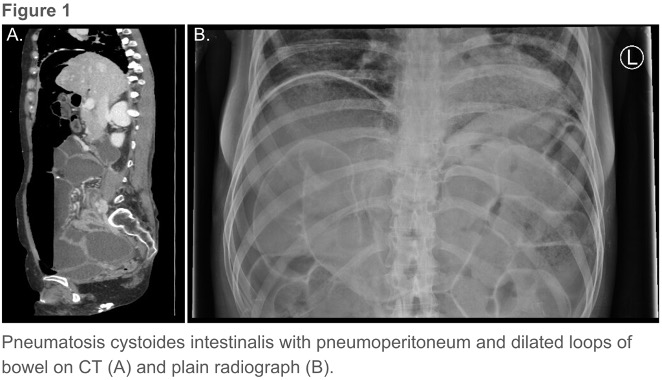
Figure: Pneumatosis cystoides intestinalis with pneumoperitoneum and dilated loops of bowel on CT (A) and plain radiograph (B).
Disclosures:
Matthew Still indicated no relevant financial relationships.
Jeevin Sandhu indicated no relevant financial relationships.
Bianca Chang indicated no relevant financial relationships.
Ali Rezaie: Ardelyx – Consultant. Bausch Health – Consultant, Speakers Bureau. Gemelli Biotech – Stock-privately held company. GoodLFE – Stock-privately held company.
Matthew Still, DO, BS1, Jeevin S. Sandhu, DO, BA2, Bianca W. Chang, MD3, Ali Rezaie, MD4. P5028 - Clearing the Air: Non-Surgical Management of Pneumatosis in Scleroderma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
