Tuesday Poster Session
Category: Small Intestine
P5030 - A Case of Autoimmune Enteropathy Associated With Lymphocytic Colitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kwabena Asafo-Agyei, MBChB
Medical College of Georgia, Augusta University
Augusta, GA
Presenting Author(s)
Kwabena Asafo-Agyei, MBChB1, Dustin Hadley, PA-C2, John Kirkikis, MD2
1Medical College of Georgia, Augusta University, Augusta, GA; 2GIS, Shreveport, LA
Introduction: Autoimmune enteropathy (AIE) is a rare pathology characterized by malabsorption, varying degrees of villous atrophy of the small intestinal mucosa, and the presence of autoantibodies to the enterocytes and goblet cells.
This disease is predominantly found in the pediatric population but is rare in the adult population and is associated with other autoimmune diseases.
However, association of this disorder with lymphocytic colitis is rare.
Case Description/Methods: A 50-year-old white female with a history of hypothyroidism was evaluated at the gastroenterology clinic with chronic diarrhea for more than 3 months.
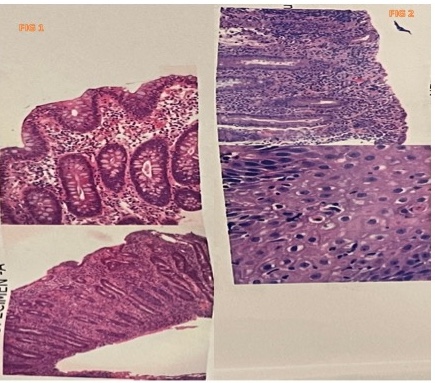
The patient initially underwent a computed tomography (CT) scan of the abdomen/pelvis, which showed fluid within the colon and distal small bowel without evidence of bowel dilatation. EGD revealed erythematous mucosa in the stomach and nonsevere reflux esophagitis. Duodenal biopsies showed marked villous blunting and partial loss of goblet and Paneth cells, with findings suspicious of celiac versus autoimmune enteropathy (Fig 1). A Positive Acid Schiff stain was negative for Whipple’s disease.
A colonoscopy showed erythematous mucosa in the distal rectum, and random biopsies were consistent with lymphocytic colitis. She was then treated with budesonide and started on a gluten-free diet without improvement of symptoms. She again underwent EGD with duodenal biopsies, which showed marked villous blunting, increased intraepithelial lymphocytes, frequent apoptotic bodies, erosions, and acute inflammation (Fig 2). The overall findings were concerning for autoimmune enteropathy. Flexible sigmoidoscopy with a colonic biopsy was unremarkable, with the subsequent celiac panel negative, normal Ig A, and the Antinuclear antibody (ANA) titer was 1:640. Celiac genetic testing with DQ haplotype testing was permissive for celiac disease (CD) but non-diagnostic.
The patient was treated with Adalimumab for AIE, and her symptoms improved.
Discussion: AIE poses a clinical diagnostic challenge as there are multiple causes of malabsorption with small bowel villous blunting, such as refractory CD, Crohn’s disease, and medication-induced enteropathy. Five criteria have been established for diagnosing adult AIE, with the first four essential for a definitive diagnosis.
AIE is due to immune dysregulation, and other autoantibodies, including ANA, may be present.
Gastroenterologists should be familiar with this rare disease and its diagnostic challenge to enhance earlier diagnosis and treatment.
Disclosures:
Kwabena Asafo-Agyei, MBChB1, Dustin Hadley, PA-C2, John Kirkikis, MD2. P5030 - A Case of Autoimmune Enteropathy Associated With Lymphocytic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Georgia, Augusta University, Augusta, GA; 2GIS, Shreveport, LA
Introduction: Autoimmune enteropathy (AIE) is a rare pathology characterized by malabsorption, varying degrees of villous atrophy of the small intestinal mucosa, and the presence of autoantibodies to the enterocytes and goblet cells.
This disease is predominantly found in the pediatric population but is rare in the adult population and is associated with other autoimmune diseases.
However, association of this disorder with lymphocytic colitis is rare.
Case Description/Methods: A 50-year-old white female with a history of hypothyroidism was evaluated at the gastroenterology clinic with chronic diarrhea for more than 3 months.
The patient initially underwent a computed tomography (CT) scan of the abdomen/pelvis, which showed fluid within the colon and distal small bowel without evidence of bowel dilatation. EGD revealed erythematous mucosa in the stomach and nonsevere reflux esophagitis. Duodenal biopsies showed marked villous blunting and partial loss of goblet and Paneth cells, with findings suspicious of celiac versus autoimmune enteropathy (Fig 1). A Positive Acid Schiff stain was negative for Whipple’s disease.
A colonoscopy showed erythematous mucosa in the distal rectum, and random biopsies were consistent with lymphocytic colitis. She was then treated with budesonide and started on a gluten-free diet without improvement of symptoms. She again underwent EGD with duodenal biopsies, which showed marked villous blunting, increased intraepithelial lymphocytes, frequent apoptotic bodies, erosions, and acute inflammation (Fig 2). The overall findings were concerning for autoimmune enteropathy. Flexible sigmoidoscopy with a colonic biopsy was unremarkable, with the subsequent celiac panel negative, normal Ig A, and the Antinuclear antibody (ANA) titer was 1:640. Celiac genetic testing with DQ haplotype testing was permissive for celiac disease (CD) but non-diagnostic.
The patient was treated with Adalimumab for AIE, and her symptoms improved.
Discussion: AIE poses a clinical diagnostic challenge as there are multiple causes of malabsorption with small bowel villous blunting, such as refractory CD, Crohn’s disease, and medication-induced enteropathy. Five criteria have been established for diagnosing adult AIE, with the first four essential for a definitive diagnosis.
AIE is due to immune dysregulation, and other autoantibodies, including ANA, may be present.
Gastroenterologists should be familiar with this rare disease and its diagnostic challenge to enhance earlier diagnosis and treatment.
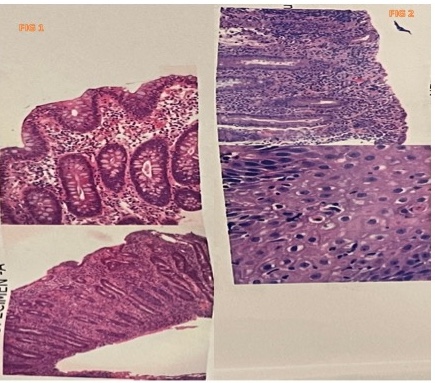
Figure: PATHOLOGY SLIDES
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
Dustin Hadley indicated no relevant financial relationships.
John Kirkikis indicated no relevant financial relationships.
Kwabena Asafo-Agyei, MBChB1, Dustin Hadley, PA-C2, John Kirkikis, MD2. P5030 - A Case of Autoimmune Enteropathy Associated With Lymphocytic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
