Tuesday Poster Session
Category: Small Intestine
P5034 - A Case of Intestinal Mycobacterium tilburgii in the Setting of Pancytopenia and Idiopathic CD4 Lymphopenia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nisha Sanghani, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Nisha Sanghani, DO1, Yemesrach D. Kerego, MD2, Michael Harring, MD3, Arianna Mesrobian, BS4, Het Patel, DO1, Kimberly Jegel. Chaput, DO5, Shaden Eldakar-Hein, MD, MS6, Russell Plowman, MD1, Berhanu Geme, MD7
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's Hospital, Bethlehem, PA; 3Saint Luke's University Hospital, Bethlehem, PA; 4Temple University, St. Luke's School of Medicine, Bethlehem, PA; 5St. Luke’s, Bethlehem, PA; 6Lewis Katz School of Medicine at Temple University, Stroudsburg, PA; 7St. Luke’s University Hospital, Center Valley, PA
Introduction: Mycobacterium tilburgii is a nontuberculous atypical mycobacterium that is implicated as an opportunistic pathogen and is rarely reported in literature. This organism is historically nonculturable, which has hindered the collection of sensitivity data to direct treatment. This is a unique case of a patient with no history of HIV who presented with vague, systemic symptoms and was eventually found to have acid-fast bacilli (AFB) in intestinal organs discovered via upper endoscopy (EGD).
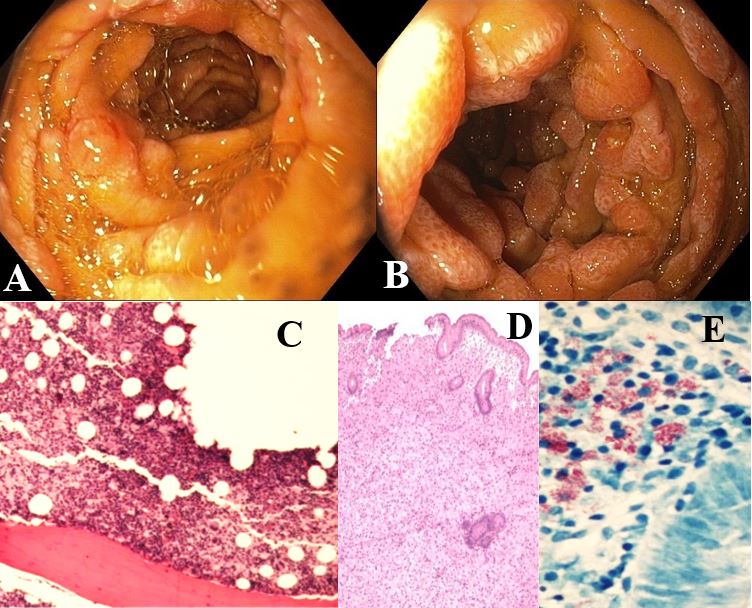
Case Description/Methods: A 67-year-old male with a history of H. pylori, eczema, reflux esophagitis, gastric ulcers, and hemorrhoids presented to a gastroenterology clinic for EGD and colonoscopy after three recent hospitalizations for fatigue, pancytopenia, and unintended weight loss. Initial hospital labs were significant for elevated alkaline phosphatase and hypoalbuminemia. A CT abdomen pelvis showed marked inflammation of the small bowel and a bone marrow (BM) biopsy showed a clonal T cell population. During endoscopies, multiple AFB were identified from biopsies obtained from the duodenum, terminal ileum, and colon, raising concern for gastrointestinal tuberculosis (TB). Subsequent BM biopsy also revealed AFB, prompting initiation of anti-TB therapy that was later modified after a PCR analysis confirmed M. tilburgii. Throughout hospitalizations, serial HIV testing was negative despite a CD4 count of 10. There was no clear explanation for his immunosuppressed state apart from upadacitinib use, which was discontinued about one year prior. Furthermore, the patient underwent a liver biopsy, which showed AFB organisms present in the portal and sinusoidal macrophages without evidence of fibrosis. One may postulate that AFB invasion of the portal vasculature could have resulted in portal hypertension, previously evidenced by a single medium type 1 isolated gastric varix. The patient was started on daily rifampin, ethambutol, azithromycin, and pyridoxine, and amikacin 3 days weekly. He has shown gradual weight gain and improved energy on medication and is now being closely monitored with outpatient care.
Discussion: Our case uniquely demonstrates that disseminated M. tilburgii can occur in an immunocompetent appearing person. This patient was found to have an extensive gastrointestinal manifestation of this rare infection. Ultimately, this case exemplifies the necessity of thorough workups and highlights the utility of a multidisciplinary approach for patients with vague clinical presentations.
Disclosures:
Nisha Sanghani, DO1, Yemesrach D. Kerego, MD2, Michael Harring, MD3, Arianna Mesrobian, BS4, Het Patel, DO1, Kimberly Jegel. Chaput, DO5, Shaden Eldakar-Hein, MD, MS6, Russell Plowman, MD1, Berhanu Geme, MD7. P5034 - A Case of Intestinal <i>Mycobacterium tilburgii</i> in the Setting of Pancytopenia and Idiopathic CD4 Lymphopenia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's Hospital, Bethlehem, PA; 3Saint Luke's University Hospital, Bethlehem, PA; 4Temple University, St. Luke's School of Medicine, Bethlehem, PA; 5St. Luke’s, Bethlehem, PA; 6Lewis Katz School of Medicine at Temple University, Stroudsburg, PA; 7St. Luke’s University Hospital, Center Valley, PA
Introduction: Mycobacterium tilburgii is a nontuberculous atypical mycobacterium that is implicated as an opportunistic pathogen and is rarely reported in literature. This organism is historically nonculturable, which has hindered the collection of sensitivity data to direct treatment. This is a unique case of a patient with no history of HIV who presented with vague, systemic symptoms and was eventually found to have acid-fast bacilli (AFB) in intestinal organs discovered via upper endoscopy (EGD).
Case Description/Methods: A 67-year-old male with a history of H. pylori, eczema, reflux esophagitis, gastric ulcers, and hemorrhoids presented to a gastroenterology clinic for EGD and colonoscopy after three recent hospitalizations for fatigue, pancytopenia, and unintended weight loss. Initial hospital labs were significant for elevated alkaline phosphatase and hypoalbuminemia. A CT abdomen pelvis showed marked inflammation of the small bowel and a bone marrow (BM) biopsy showed a clonal T cell population. During endoscopies, multiple AFB were identified from biopsies obtained from the duodenum, terminal ileum, and colon, raising concern for gastrointestinal tuberculosis (TB). Subsequent BM biopsy also revealed AFB, prompting initiation of anti-TB therapy that was later modified after a PCR analysis confirmed M. tilburgii. Throughout hospitalizations, serial HIV testing was negative despite a CD4 count of 10. There was no clear explanation for his immunosuppressed state apart from upadacitinib use, which was discontinued about one year prior. Furthermore, the patient underwent a liver biopsy, which showed AFB organisms present in the portal and sinusoidal macrophages without evidence of fibrosis. One may postulate that AFB invasion of the portal vasculature could have resulted in portal hypertension, previously evidenced by a single medium type 1 isolated gastric varix. The patient was started on daily rifampin, ethambutol, azithromycin, and pyridoxine, and amikacin 3 days weekly. He has shown gradual weight gain and improved energy on medication and is now being closely monitored with outpatient care.
Discussion: Our case uniquely demonstrates that disseminated M. tilburgii can occur in an immunocompetent appearing person. This patient was found to have an extensive gastrointestinal manifestation of this rare infection. Ultimately, this case exemplifies the necessity of thorough workups and highlights the utility of a multidisciplinary approach for patients with vague clinical presentations.
Figure: A-B. Endoscopic images displaying severe edematous and nodular mucosa in the 2nd and 3rd parts of the duodenum.
C. High power image of the patient’s bone marrow. Diffuse sheets of large polyhedral finely granular histiocytes (macrophages) with rare faint foci of granulomatous pattern. H&E 400X.
D. A diffuse/expansive histiocytic infiltration of the lamina propria. H&E 100X.
E. AFB filling the cytoplasm of the macrophage. Infiltrate in the lamina propria. AFB STAIN 400X.
C. High power image of the patient’s bone marrow. Diffuse sheets of large polyhedral finely granular histiocytes (macrophages) with rare faint foci of granulomatous pattern. H&E 400X.
D. A diffuse/expansive histiocytic infiltration of the lamina propria. H&E 100X.
E. AFB filling the cytoplasm of the macrophage. Infiltrate in the lamina propria. AFB STAIN 400X.
Disclosures:
Nisha Sanghani indicated no relevant financial relationships.
Yemesrach Kerego indicated no relevant financial relationships.
Michael Harring indicated no relevant financial relationships.
Arianna Mesrobian indicated no relevant financial relationships.
Het Patel indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Shaden Eldakar-Hein indicated no relevant financial relationships.
Russell Plowman indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Nisha Sanghani, DO1, Yemesrach D. Kerego, MD2, Michael Harring, MD3, Arianna Mesrobian, BS4, Het Patel, DO1, Kimberly Jegel. Chaput, DO5, Shaden Eldakar-Hein, MD, MS6, Russell Plowman, MD1, Berhanu Geme, MD7. P5034 - A Case of Intestinal <i>Mycobacterium tilburgii</i> in the Setting of Pancytopenia and Idiopathic CD4 Lymphopenia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

