Tuesday Poster Session
Category: Stomach
P5040 - Trends and Disparities in Peptic Ulcer Disease-Related Mortality Among Adults in the United States: An Analysis of 22 Years
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Usama Qamar, MD
King Edward Medical University
Rochester, MN
Presenting Author(s)
Usama Qamar, MD1, Aamir Saeed, MD2, Waleed Qamar, MBBS1, Sarosh A. Khan, MD3, Sultan Mahmood, MD4, Ijlal Akbar Ali, MD5
1King Edward Medical University, Lahore, Punjab, Pakistan; 2Vanderbilt University Medical Center, Nashville, TN; 3Integris Baptist Medical Center, Oklahoma City, OK; 4University of Pittsburgh Medical Center, Pittsburgh, PA; 5University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Peptic Ulcer Disease (PUD) has a high prevalence in the United States (US) but its associated mortality patterns have not been studied well. This study aims to determine PUD-related mortality trends from 1999 to 2020 among adults in the United States.
Methods: We used Data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database to retrieve statistics from all the death certificates where PUD was listed as an underlying or contributing cause of death. Age-adjusted mortality rates (AAMRs) per 1 million individuals were calculated and the Joinpoint regression model was used to elucidate longitudinal mortality patterns by determining annual percent change (APC) in AAMRs.
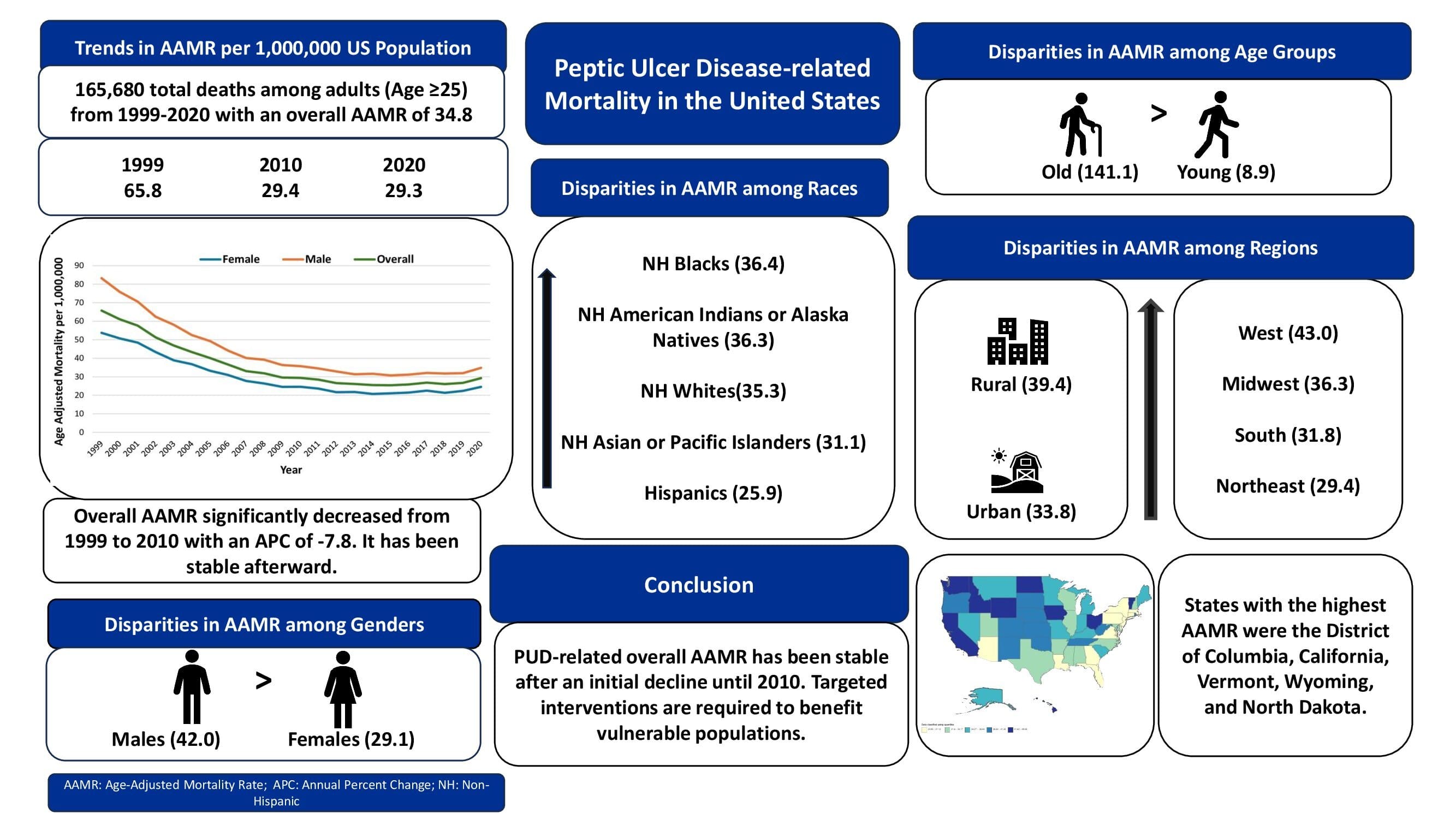
Results: There was a total of 165,680 PUD-related deaths among adults aged ≥25 years in the US between 1999 and 2020, with a cumulative overall AAMR of 34.8. The overall AAMR declined significantly from 1999-2010 (APC: -7.8; p< 0.01) and has been stable afterward till 2020 (APC: -0.03; p=0.92). Males had higher cumulative AAMR than females (42.0 vs 29.1, respectively). AAMR in males followed the same trend as overall AAMR; AAMR in females declined significantly till 2012 (APC: -7.2; p< 0.01) and then significantly increased till 2020 (APC: 1.6; p< 0.05). Older adults aged ≥65 years (141.1) had much higher cumulative AAMR than younger adults aged 25-64 years (8.9). Among races, Non-Hispanic (NH) Blacks/African Americans had the highest cumulative AAMR (36.4), followed by NH American Indians/Alaska Natives (36.3), NH Whites (35.3), NH Asians/Pacific Islanders (31.1), and Hispanics/Latinos (25.9). Rural areas had higher AAMR than urban areas (39.4 vs 33.8, respectively). AAMR varied substantially across states from 23.9 in Massachusetts to 45.5 in the District of Columbia (Central illustration). The West region had the highest cumulative AAMR (43.0), followed by the Midwest (36.3), South (31.8), and Northeast (29.4) regions.
Discussion: PUD-related overall AAMR has been stable after an initial decline until 2010. Higher mortality rates were observed among males, NH Blacks, elderly, and residents of rural areas and the West region. Disparities observed in our study may arise from differences in the availability of gastroenterologists, healthcare quality, and socioeconomic and behavioral factors. Effective public health strategies are required to benefit vulnerable populations.
Disclosures:
Usama Qamar, MD1, Aamir Saeed, MD2, Waleed Qamar, MBBS1, Sarosh A. Khan, MD3, Sultan Mahmood, MD4, Ijlal Akbar Ali, MD5. P5040 - Trends and Disparities in Peptic Ulcer Disease-Related Mortality Among Adults in the United States: An Analysis of 22 Years, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1King Edward Medical University, Lahore, Punjab, Pakistan; 2Vanderbilt University Medical Center, Nashville, TN; 3Integris Baptist Medical Center, Oklahoma City, OK; 4University of Pittsburgh Medical Center, Pittsburgh, PA; 5University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Peptic Ulcer Disease (PUD) has a high prevalence in the United States (US) but its associated mortality patterns have not been studied well. This study aims to determine PUD-related mortality trends from 1999 to 2020 among adults in the United States.
Methods: We used Data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database to retrieve statistics from all the death certificates where PUD was listed as an underlying or contributing cause of death. Age-adjusted mortality rates (AAMRs) per 1 million individuals were calculated and the Joinpoint regression model was used to elucidate longitudinal mortality patterns by determining annual percent change (APC) in AAMRs.
Results: There was a total of 165,680 PUD-related deaths among adults aged ≥25 years in the US between 1999 and 2020, with a cumulative overall AAMR of 34.8. The overall AAMR declined significantly from 1999-2010 (APC: -7.8; p< 0.01) and has been stable afterward till 2020 (APC: -0.03; p=0.92). Males had higher cumulative AAMR than females (42.0 vs 29.1, respectively). AAMR in males followed the same trend as overall AAMR; AAMR in females declined significantly till 2012 (APC: -7.2; p< 0.01) and then significantly increased till 2020 (APC: 1.6; p< 0.05). Older adults aged ≥65 years (141.1) had much higher cumulative AAMR than younger adults aged 25-64 years (8.9). Among races, Non-Hispanic (NH) Blacks/African Americans had the highest cumulative AAMR (36.4), followed by NH American Indians/Alaska Natives (36.3), NH Whites (35.3), NH Asians/Pacific Islanders (31.1), and Hispanics/Latinos (25.9). Rural areas had higher AAMR than urban areas (39.4 vs 33.8, respectively). AAMR varied substantially across states from 23.9 in Massachusetts to 45.5 in the District of Columbia (Central illustration). The West region had the highest cumulative AAMR (43.0), followed by the Midwest (36.3), South (31.8), and Northeast (29.4) regions.
Discussion: PUD-related overall AAMR has been stable after an initial decline until 2010. Higher mortality rates were observed among males, NH Blacks, elderly, and residents of rural areas and the West region. Disparities observed in our study may arise from differences in the availability of gastroenterologists, healthcare quality, and socioeconomic and behavioral factors. Effective public health strategies are required to benefit vulnerable populations.
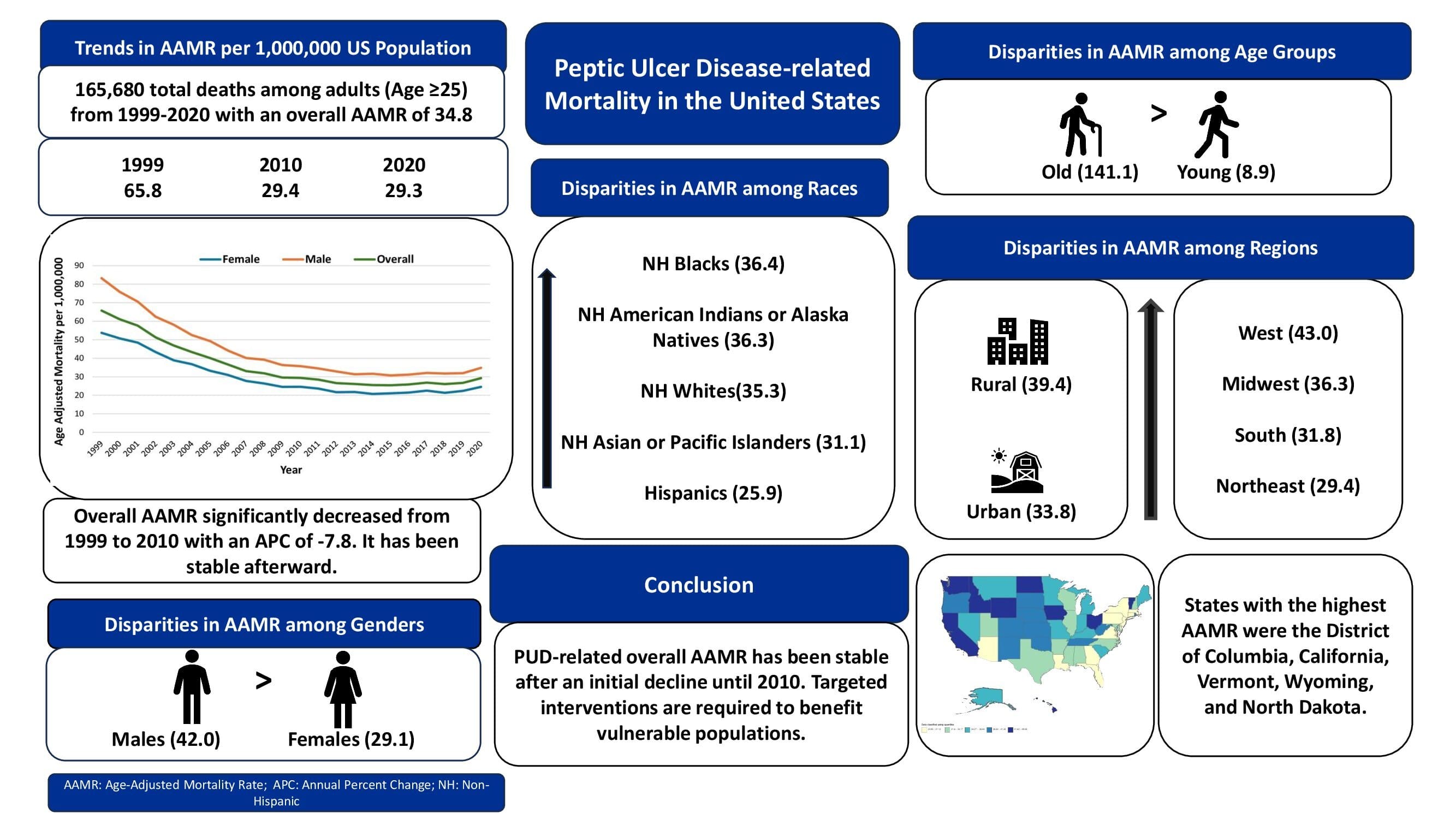
Figure: Peptic Ulcer Disease-related Mortality Among Adults in the United States, 1999-2020.
Disclosures:
Usama Qamar indicated no relevant financial relationships.
Aamir Saeed indicated no relevant financial relationships.
Waleed Qamar indicated no relevant financial relationships.
Sarosh Khan indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Ijlal Akbar Ali indicated no relevant financial relationships.
Usama Qamar, MD1, Aamir Saeed, MD2, Waleed Qamar, MBBS1, Sarosh A. Khan, MD3, Sultan Mahmood, MD4, Ijlal Akbar Ali, MD5. P5040 - Trends and Disparities in Peptic Ulcer Disease-Related Mortality Among Adults in the United States: An Analysis of 22 Years, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
