Tuesday Poster Session
Category: Stomach
P5043 - A Resident-Led Project to Improve Education and Standardize Post-Procedural Care of Endoscopically Placed Gastrostomy Tubes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Priyanka Jagannathan, MD
University of Texas at Austin Dell Medical School
Austin, TX
Presenting Author(s)
Priyanka Jagannathan, MD, Sara Gottesman, MD, Christoffer Lam, MD, Vincent Phan, MD, Faraz Jafri, MD, Sagarika Satyavada, MD
University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Patients with recent gastrostomy tube placements are at increased risk for dislodgements, delayed re-initiation of nutrition, and more severe adverse events. Many such events are related to dressing care and lack of information. This project aims to improve knowledge and comfort on post-procedural management of percutaneous endoscopic gastrostomy (PEG) tubes for internal medicine residents and nursing staff.
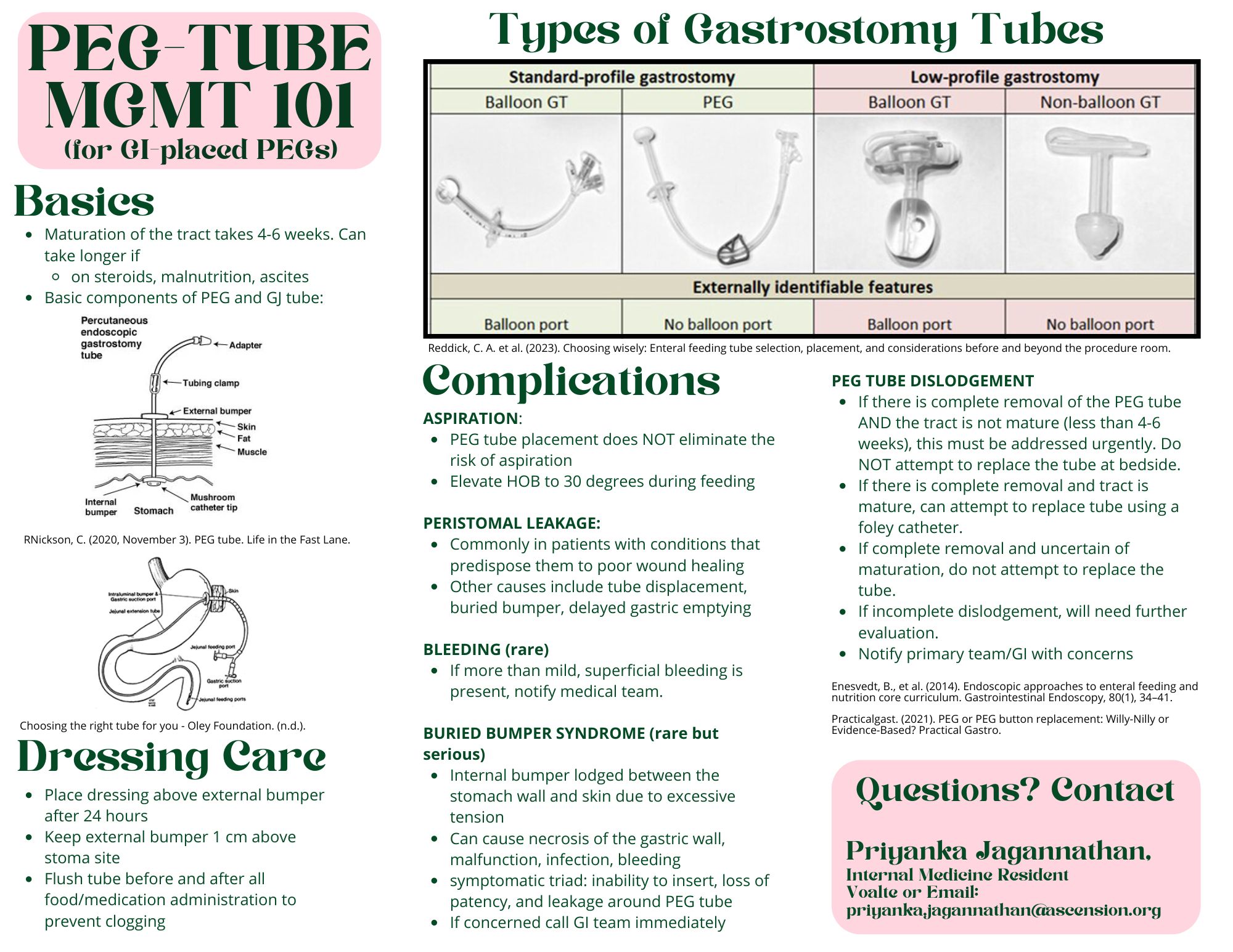
Methods: We created a standardized dot phrase that was documented at the end of PEG tube procedural notes detailing dressing and nutrition recommendations. Residents and nursing staff received a formal 30-minute lecture either during didactics or huddle, respectively. A summative one-pager (Figure A) was then distributed through the chief residents and nursing education coordinators. PEG tube knowledge and comfort in identifying and managing complications were assessed via a pre- and 2-week post- intervention survey.
Results: In the 10 PEGs placed during the intervention period, there was a 90% adoption rate of the dot phrase. A 94% increase in the inclusion of dressing recommendations in gastroenterology (GI) documentation was seen. There was a 200% increase in formal recommendations provided by the nutrition service within 24 hours of PEG placement.
Survey results generally showed improvement in comfort in management of PEG tubes in the peri-procedural period. Specifically, confidence in ability to manage a dislodged PEG by residents improved from a median of 1 (strongly disagree) to 4.5 (strongly agree) with a p-value < 0.001. Self-reported understanding of how dressing changes impact risk for complications improved from a median of 1.5 (strongly disagree) to 5 (strongly agree) for nursing staff (p-value < 0.001).
Discussion: Through didactic sessions and streamlined access to formal recommendations, we were able to improve the comfort of PEG tube management in our target population. Our intervention not only increased the dissemination of information but also increased follow-up recommendations from the nutrition service. This educational intervention may have an impact on PEG tube-related complications. Future studies could further investigate these outcomes.
Disclosures:
Priyanka Jagannathan, MD, Sara Gottesman, MD, Christoffer Lam, MD, Vincent Phan, MD, Faraz Jafri, MD, Sagarika Satyavada, MD. P5043 - A Resident-Led Project to Improve Education and Standardize Post-Procedural Care of Endoscopically Placed Gastrostomy Tubes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Patients with recent gastrostomy tube placements are at increased risk for dislodgements, delayed re-initiation of nutrition, and more severe adverse events. Many such events are related to dressing care and lack of information. This project aims to improve knowledge and comfort on post-procedural management of percutaneous endoscopic gastrostomy (PEG) tubes for internal medicine residents and nursing staff.
Methods: We created a standardized dot phrase that was documented at the end of PEG tube procedural notes detailing dressing and nutrition recommendations. Residents and nursing staff received a formal 30-minute lecture either during didactics or huddle, respectively. A summative one-pager (Figure A) was then distributed through the chief residents and nursing education coordinators. PEG tube knowledge and comfort in identifying and managing complications were assessed via a pre- and 2-week post- intervention survey.
Results: In the 10 PEGs placed during the intervention period, there was a 90% adoption rate of the dot phrase. A 94% increase in the inclusion of dressing recommendations in gastroenterology (GI) documentation was seen. There was a 200% increase in formal recommendations provided by the nutrition service within 24 hours of PEG placement.
Survey results generally showed improvement in comfort in management of PEG tubes in the peri-procedural period. Specifically, confidence in ability to manage a dislodged PEG by residents improved from a median of 1 (strongly disagree) to 4.5 (strongly agree) with a p-value < 0.001. Self-reported understanding of how dressing changes impact risk for complications improved from a median of 1.5 (strongly disagree) to 5 (strongly agree) for nursing staff (p-value < 0.001).
Discussion: Through didactic sessions and streamlined access to formal recommendations, we were able to improve the comfort of PEG tube management in our target population. Our intervention not only increased the dissemination of information but also increased follow-up recommendations from the nutrition service. This educational intervention may have an impact on PEG tube-related complications. Future studies could further investigate these outcomes.
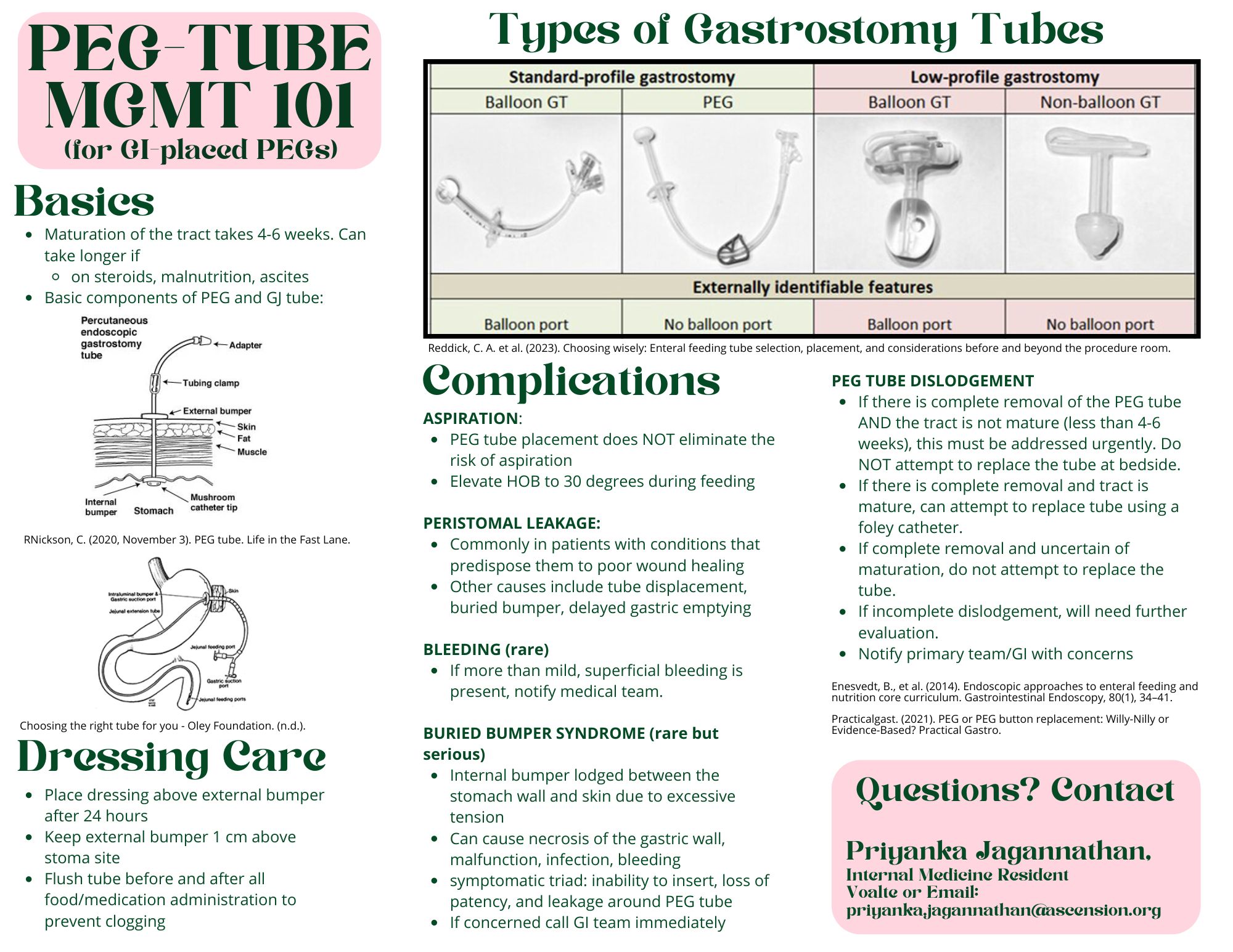
Figure: PEG Tube Management One-Page Summary
Disclosures:
Priyanka Jagannathan indicated no relevant financial relationships.
Sara Gottesman indicated no relevant financial relationships.
Christoffer Lam indicated no relevant financial relationships.
Vincent Phan indicated no relevant financial relationships.
Faraz Jafri indicated no relevant financial relationships.
Sagarika Satyavada indicated no relevant financial relationships.
Priyanka Jagannathan, MD, Sara Gottesman, MD, Christoffer Lam, MD, Vincent Phan, MD, Faraz Jafri, MD, Sagarika Satyavada, MD. P5043 - A Resident-Led Project to Improve Education and Standardize Post-Procedural Care of Endoscopically Placed Gastrostomy Tubes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
