Tuesday Poster Session
Category: Stomach
P5114 - Mega-Stomach and a Gastric Atony as an Initial Presentation of Systemic Amyloidosis: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Akram Ahmad, MD
Cleveland Clinic Florida
Weston, FL
Presenting Author(s)
Akram Ahmad, MD1, Isabella Suarez Alcala, MD2, Natasha Mederos, MD3, Adrianna Wierzbicka, MD1, Zaid Ansari, MD4, Emanuele Lo Menzo, MD1, Andrew Ukleja, MD1
1Cleveland Clinic Florida, Weston, FL; 2Palmetto General Hospital, Hialeah, FL; 3University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 4Cleveland Clinic Florida, Plantation, FL
Introduction: Amyloidosis of the gastrointestinal (GI) tract may be limited to the gut or part of systemic involvement.
The accumulative deposition of misfolded proteins characterizes Amyloidosis. GI amyloidosis is defined by GI symptoms (abdominal pain, dyspepsia, diarrhea, weight loss, or GI bleeding) and biopsy-proven amyloid involvement in the GI tract. We present a case of a patient labelled as diabetic gastroparesis, who was later found to have mega-stomach and upper GI bleeding related to AL amyloidosis.
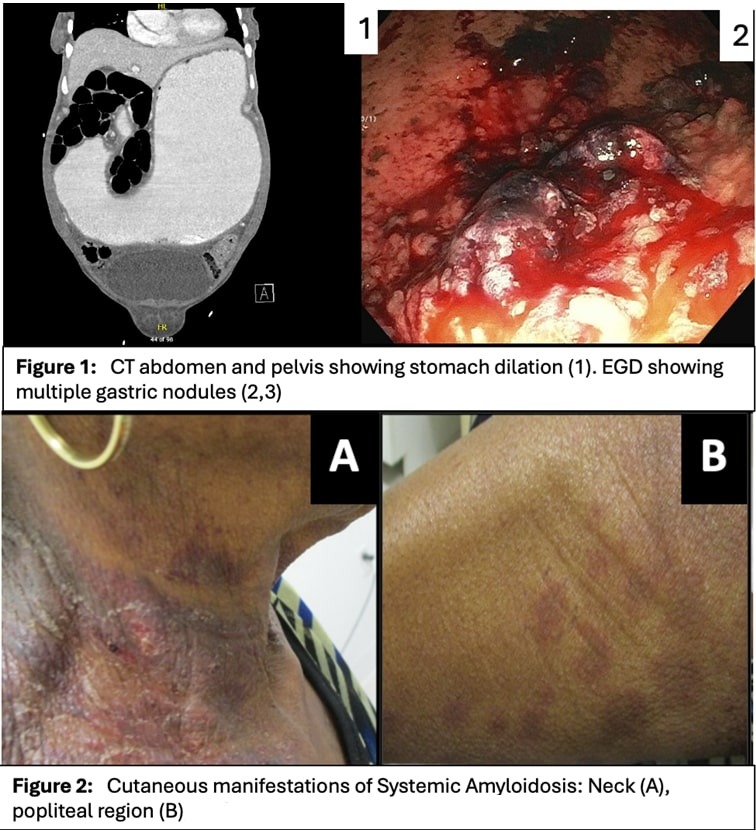
Case Description/Methods: A 71-year-old female with diabetes mellitus, rheumatoid arthritis, and gastroparesis presented to the emergency department with nausea, vomiting, and weight loss of 60 lbs. Her outside GI workup included EGD, which showed a large amount of food residue and gastric biopsies positive for Helicobacter pylori. A gastric scintigraphy revealed 89% gastric retention at 4 hrs, consistent with severe gastroparesis. On admission, a CT scan of the abdomen/pelvis showed a massively dilated stomach [Figure 1 (1)]. She was found to have a hemoglobin level of 6 g/dL and melena consistent with upper GI bleeding. EGD revealed a copious amount of heme, nodular mucosa, and a dilated stomach [Figure 1 (2,3)]. Gastric biopsies were positive for Congo red, and thioflavin S stains confirmed amyloidosis. The patient required frequent blood transfusions due to ongoing upper GI bleeding. Because of refractory GI bleeding, a total gastrectomy with Roux-en-Y esophagojejunostomy was performed. Histologic specimen confirmed amyloidosis involving all layers of the stomach wall. Later, she developed systemic involvement with cutaneous nodular amyloidosis (Figure 2), nephrotic-range proteinuria, and myocardial changes. A bone marrow biopsy revealed multiple myeloma with systemic AL amyloidosis.
Discussion: This case underscores the complexity of diagnosing systemic amyloidosis when initial symptoms can mimic other conditions, in our case, gastroparesis. The diagnosis of amyloidosis was delayed since the initial gastric biopsies were not stained for Congo red. The patient required gastrectomy due to gastric atony and diffuse uncontrollable GI bleeding. Treatment typically focuses on reducing amyloid protein formation through chemotherapy or radiation. However, some cases may require surgical intervention to manage refractory symptoms and improve overall outcomes.
Disclosures:
Akram Ahmad, MD1, Isabella Suarez Alcala, MD2, Natasha Mederos, MD3, Adrianna Wierzbicka, MD1, Zaid Ansari, MD4, Emanuele Lo Menzo, MD1, Andrew Ukleja, MD1. P5114 - Mega-Stomach and a Gastric Atony as an Initial Presentation of Systemic Amyloidosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Florida, Weston, FL; 2Palmetto General Hospital, Hialeah, FL; 3University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 4Cleveland Clinic Florida, Plantation, FL
Introduction: Amyloidosis of the gastrointestinal (GI) tract may be limited to the gut or part of systemic involvement.
The accumulative deposition of misfolded proteins characterizes Amyloidosis. GI amyloidosis is defined by GI symptoms (abdominal pain, dyspepsia, diarrhea, weight loss, or GI bleeding) and biopsy-proven amyloid involvement in the GI tract. We present a case of a patient labelled as diabetic gastroparesis, who was later found to have mega-stomach and upper GI bleeding related to AL amyloidosis.
Case Description/Methods: A 71-year-old female with diabetes mellitus, rheumatoid arthritis, and gastroparesis presented to the emergency department with nausea, vomiting, and weight loss of 60 lbs. Her outside GI workup included EGD, which showed a large amount of food residue and gastric biopsies positive for Helicobacter pylori. A gastric scintigraphy revealed 89% gastric retention at 4 hrs, consistent with severe gastroparesis. On admission, a CT scan of the abdomen/pelvis showed a massively dilated stomach [Figure 1 (1)]. She was found to have a hemoglobin level of 6 g/dL and melena consistent with upper GI bleeding. EGD revealed a copious amount of heme, nodular mucosa, and a dilated stomach [Figure 1 (2,3)]. Gastric biopsies were positive for Congo red, and thioflavin S stains confirmed amyloidosis. The patient required frequent blood transfusions due to ongoing upper GI bleeding. Because of refractory GI bleeding, a total gastrectomy with Roux-en-Y esophagojejunostomy was performed. Histologic specimen confirmed amyloidosis involving all layers of the stomach wall. Later, she developed systemic involvement with cutaneous nodular amyloidosis (Figure 2), nephrotic-range proteinuria, and myocardial changes. A bone marrow biopsy revealed multiple myeloma with systemic AL amyloidosis.
Discussion: This case underscores the complexity of diagnosing systemic amyloidosis when initial symptoms can mimic other conditions, in our case, gastroparesis. The diagnosis of amyloidosis was delayed since the initial gastric biopsies were not stained for Congo red. The patient required gastrectomy due to gastric atony and diffuse uncontrollable GI bleeding. Treatment typically focuses on reducing amyloid protein formation through chemotherapy or radiation. However, some cases may require surgical intervention to manage refractory symptoms and improve overall outcomes.
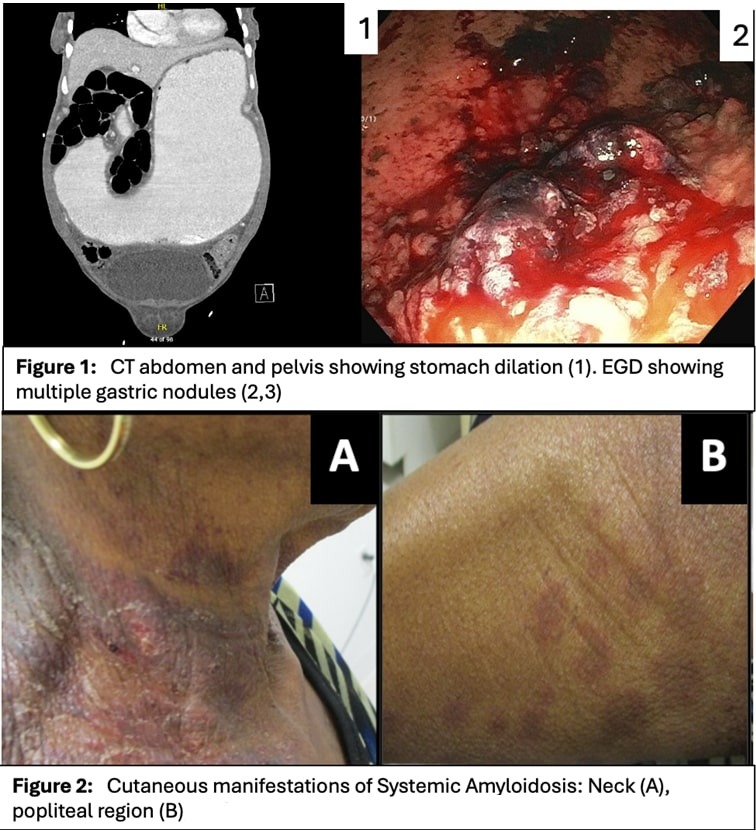
Figure: Figure 1
Disclosures:
Akram Ahmad indicated no relevant financial relationships.
Isabella Suarez Alcala indicated no relevant financial relationships.
Natasha Mederos indicated no relevant financial relationships.
Adrianna Wierzbicka indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Emanuele Lo Menzo indicated no relevant financial relationships.
Andrew Ukleja indicated no relevant financial relationships.
Akram Ahmad, MD1, Isabella Suarez Alcala, MD2, Natasha Mederos, MD3, Adrianna Wierzbicka, MD1, Zaid Ansari, MD4, Emanuele Lo Menzo, MD1, Andrew Ukleja, MD1. P5114 - Mega-Stomach and a Gastric Atony as an Initial Presentation of Systemic Amyloidosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
