Tuesday Poster Session
Category: Stomach
P5129 - Exploring Acquired Double Pylorus: Insights From Two Case Studies
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- EL
Emily Liu, MD
New York Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Emily Liu, MD1, Anas Zaher, MD2, Harsh Patel, MD2, Samiaa Faruqui, MD3
1New York Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 3New York Brooklyn Methodist Hospital, Elmhurst, NY
Introduction: A double pylorus (DP) is a rare finding characterized as two channels connecting the prepyloric antrum to the duodenal bulb, reported in 0.001% to 0.4% of all endoscopies performed. Studies have shown that diabetes mellitus, sarcoidosis or rheumatoid arthritis (RA) can play a role in the development of DP by damaging the mucosal microcirculation which can lead to breakdown of the stomach lumen eventually leading to a fistula. These are usually asymptomatic and are found incidentally on esophagogastroduodenoscopy (EGD). . In this report, we describe two cases of double pylorus found during EGD.
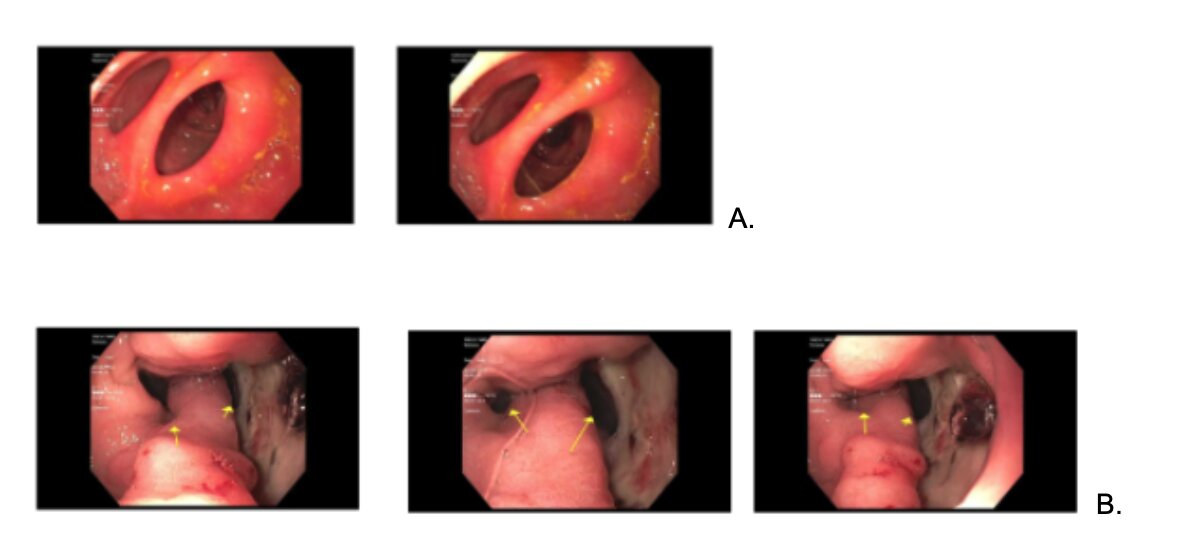
Case Description/Methods: Case 1: A 72-year-male African American (AA) with past medical history (PMH) of hypertension, RA and sarcoidosis presented to the gastroenterology clinic for further evaluation of iron deficiency anemia. He underwent EGD which showed two lumens at the site of the pylorus and both leading to the duodenum. The patient had scattered moderate inflammation and erosions in the gastric body (fig. 1) The endoscopic biopsy of the stomach was positive for chronic nonspecific gastritis and PPI was initiated.
Case 2: A 79-year-woman AA with a PMH of hypertension and previously gastric ulcer diagnosed 3 years prior presented to the ED with black stool. Hemoglobin was lower than baseline. The patient underwent an EGD due to the concern for upper gastrointestinal bleeding which revealed a large visible ulcer in the gastric antrum. In addition, there was evidence of a fistulous tract leading into the duodenal bulb. Septation was present with edematous tissue separating the two lumens leading into the duodenum (fig. 2) and was started on pantoprazole and sucralfate.
Discussion: DP can be congenital or acquired. Congenital causes of DP occur during the early stages of embryonic development usually with normal mucosa on EGD. Acquired DP are most often seen in patients with peptic ulcer disease, gastritis or gastric cancers. In case 1, the patient suffered from sarcoidosis and RA which had been correlated with developments of delayed and poor healing gastric ulcers. In case 2, the patient presented with a prominent gastric ulcer that likely led to the formation of the second lumen. DP does not present with a specific clinical symptom. Complication of DP can include gastric outlet obstruction. Treatment typically involves preventing the underlying causes with gastrointestinal acid suppression. Patients are recommended to follow up for repeat EGD to monitor for changes in the morphology of the DP.
Disclosures:
Emily Liu, MD1, Anas Zaher, MD2, Harsh Patel, MD2, Samiaa Faruqui, MD3. P5129 - Exploring Acquired Double Pylorus: Insights From Two Case Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 3New York Brooklyn Methodist Hospital, Elmhurst, NY
Introduction: A double pylorus (DP) is a rare finding characterized as two channels connecting the prepyloric antrum to the duodenal bulb, reported in 0.001% to 0.4% of all endoscopies performed. Studies have shown that diabetes mellitus, sarcoidosis or rheumatoid arthritis (RA) can play a role in the development of DP by damaging the mucosal microcirculation which can lead to breakdown of the stomach lumen eventually leading to a fistula. These are usually asymptomatic and are found incidentally on esophagogastroduodenoscopy (EGD). . In this report, we describe two cases of double pylorus found during EGD.
Case Description/Methods: Case 1: A 72-year-male African American (AA) with past medical history (PMH) of hypertension, RA and sarcoidosis presented to the gastroenterology clinic for further evaluation of iron deficiency anemia. He underwent EGD which showed two lumens at the site of the pylorus and both leading to the duodenum. The patient had scattered moderate inflammation and erosions in the gastric body (fig. 1) The endoscopic biopsy of the stomach was positive for chronic nonspecific gastritis and PPI was initiated.
Case 2: A 79-year-woman AA with a PMH of hypertension and previously gastric ulcer diagnosed 3 years prior presented to the ED with black stool. Hemoglobin was lower than baseline. The patient underwent an EGD due to the concern for upper gastrointestinal bleeding which revealed a large visible ulcer in the gastric antrum. In addition, there was evidence of a fistulous tract leading into the duodenal bulb. Septation was present with edematous tissue separating the two lumens leading into the duodenum (fig. 2) and was started on pantoprazole and sucralfate.
Discussion: DP can be congenital or acquired. Congenital causes of DP occur during the early stages of embryonic development usually with normal mucosa on EGD. Acquired DP are most often seen in patients with peptic ulcer disease, gastritis or gastric cancers. In case 1, the patient suffered from sarcoidosis and RA which had been correlated with developments of delayed and poor healing gastric ulcers. In case 2, the patient presented with a prominent gastric ulcer that likely led to the formation of the second lumen. DP does not present with a specific clinical symptom. Complication of DP can include gastric outlet obstruction. Treatment typically involves preventing the underlying causes with gastrointestinal acid suppression. Patients are recommended to follow up for repeat EGD to monitor for changes in the morphology of the DP.
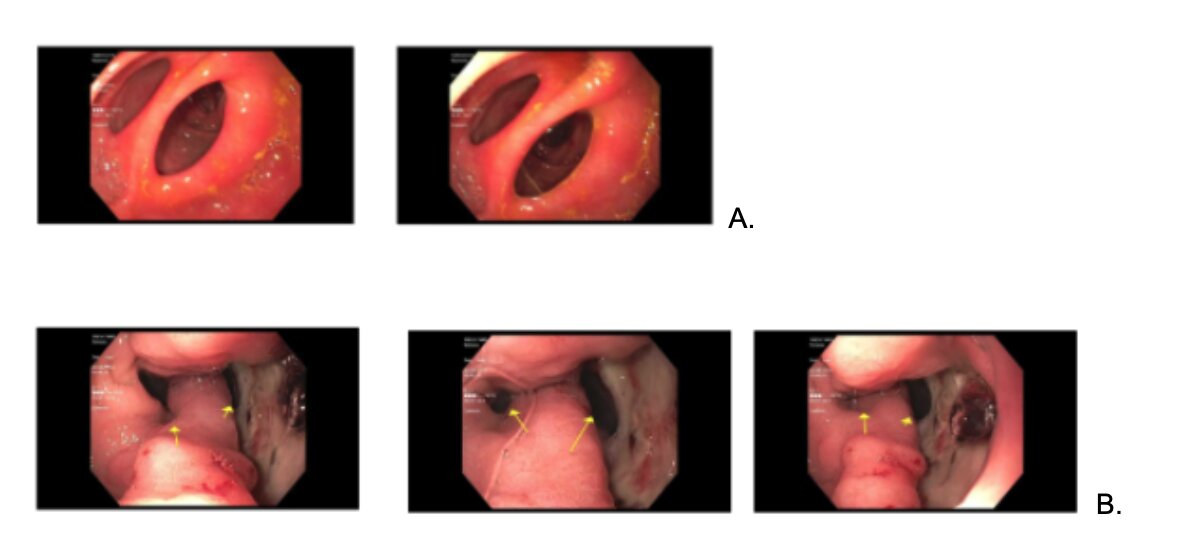
Figure: Figure A. Double pylorus is shown, leading into the duodenum. Moderate inflammation with congestion is noted.
Figure B. Two lumens leading into the duodenal bulb are shown (yellow arrows). Septation is present with edematous tissue separating the two openings into the duodenum.
Figure B. Two lumens leading into the duodenal bulb are shown (yellow arrows). Septation is present with edematous tissue separating the two openings into the duodenum.
Disclosures:
Emily Liu indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Harsh Patel indicated no relevant financial relationships.
Samiaa Faruqui indicated no relevant financial relationships.
Emily Liu, MD1, Anas Zaher, MD2, Harsh Patel, MD2, Samiaa Faruqui, MD3. P5129 - Exploring Acquired Double Pylorus: Insights From Two Case Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
