Tuesday Poster Session
Category: Stomach
P5071 - Gastric Plexiform Fibromyxoma Associated With Secondary Hypertension: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Megan Costello, BA
University of Missouri Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Megan Costello, BA1, Lavina Thadani, 1, Vinay Jahagirdar, MD1, Erin Algeo, DO1, Jason Singh, DO2, John Campbell, MD1
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2KC Pathology, Kansas City, KS
Introduction: Gastric plexiform fibromyxoma (PF) is a rare mesenchymal tumor of the stomach. It can manifest in a wide array of gastrointestinal symptoms posing a diagnostic challenge due to its nonspecific presentation. Patients may experience symptoms such as abdominal discomfort, mild abdominal distension, melena, and anemia, which can vary in severity and duration. Gastric PF is rare, with less than 150 cases described in literature.
Case Description/Methods: A 31-year-old female presented to the clinic with syncopal symptoms. She was diagnosed with hypertension in her mid-twenties, and it was managed on three agents.
She reported a family history of early onset hypertension in several relatives. Her BMI was 23.5, and she scored low on the Epworth sleepiness scale, making obstructive sleep apnea less likely. As part of the work up for secondary hypertension, renin, aldosterone, 24 hour 5-HIAA, metanephrines, normetanephrines and TSH levels were obtained and were within normal limits. Renal artery doppler velocities were not significant for stenosis.
CT-abdomen revealed a 4 cm vascular mass abutting the greater curvature of the stomach. Serum chromogranin A level was within normal limits.
On EGD, the origin of the mass was unclear as the mass could not be visualized from the lumen. On EUS, the mass appeared to have internal vascularity and heterogeneous appearance possibly consistent with necrosis. GI stromal tumor (GIST) or a neuroendocrine tumor were considered as differentials. Fine needle aspiration suggested a “spindle cell lesion,”. The slides were sent to a referral center for a second opinion, which reported a “Myxoid lesion with bland cytologic features and prominent delicate vasculature, most suggestive of PF”. Tumor markers on pathology were consistent with PF. The patient underwent surgical resection without complication. Within weeks of resection, the patient's blood pressure improved and she no longer required multiple agents.
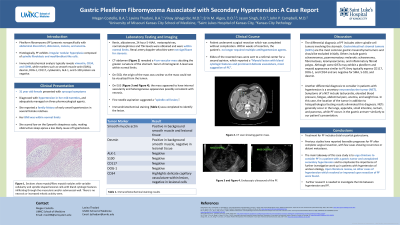
Discussion: Given its rarity and non-specific symptoms, gastric PF is often misdiagnosed as GIST. Immunohistochemical analysis typically reveals positivity for vimentin, CD34, and SDHB, which helps differentiate it from GIST. Gastric PF is managed through resection, typically performed as distal or partial gastrectomy.
Disclosures:
Megan Costello, BA1, Lavina Thadani, 1, Vinay Jahagirdar, MD1, Erin Algeo, DO1, Jason Singh, DO2, John Campbell, MD1. P5071 - Gastric Plexiform Fibromyxoma Associated With Secondary Hypertension: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri Kansas City School of Medicine, Kansas City, MO; 2KC Pathology, Kansas City, KS
Introduction: Gastric plexiform fibromyxoma (PF) is a rare mesenchymal tumor of the stomach. It can manifest in a wide array of gastrointestinal symptoms posing a diagnostic challenge due to its nonspecific presentation. Patients may experience symptoms such as abdominal discomfort, mild abdominal distension, melena, and anemia, which can vary in severity and duration. Gastric PF is rare, with less than 150 cases described in literature.
Case Description/Methods: A 31-year-old female presented to the clinic with syncopal symptoms. She was diagnosed with hypertension in her mid-twenties, and it was managed on three agents.
She reported a family history of early onset hypertension in several relatives. Her BMI was 23.5, and she scored low on the Epworth sleepiness scale, making obstructive sleep apnea less likely. As part of the work up for secondary hypertension, renin, aldosterone, 24 hour 5-HIAA, metanephrines, normetanephrines and TSH levels were obtained and were within normal limits. Renal artery doppler velocities were not significant for stenosis.
CT-abdomen revealed a 4 cm vascular mass abutting the greater curvature of the stomach. Serum chromogranin A level was within normal limits.
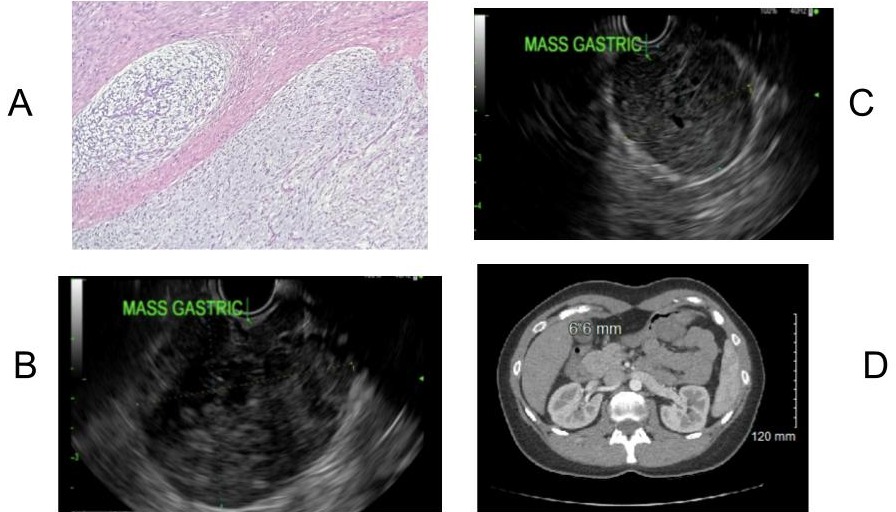
On EGD, the origin of the mass was unclear as the mass could not be visualized from the lumen. On EUS, the mass appeared to have internal vascularity and heterogeneous appearance possibly consistent with necrosis. GI stromal tumor (GIST) or a neuroendocrine tumor were considered as differentials. Fine needle aspiration suggested a “spindle cell lesion,”. The slides were sent to a referral center for a second opinion, which reported a “Myxoid lesion with bland cytologic features and prominent delicate vasculature, most suggestive of PF”. Tumor markers on pathology were consistent with PF. The patient underwent surgical resection without complication. Within weeks of resection, the patient's blood pressure improved and she no longer required multiple agents.
Discussion: Given its rarity and non-specific symptoms, gastric PF is often misdiagnosed as GIST. Immunohistochemical analysis typically reveals positivity for vimentin, CD34, and SDHB, which helps differentiate it from GIST. Gastric PF is managed through resection, typically performed as distal or partial gastrectomy.
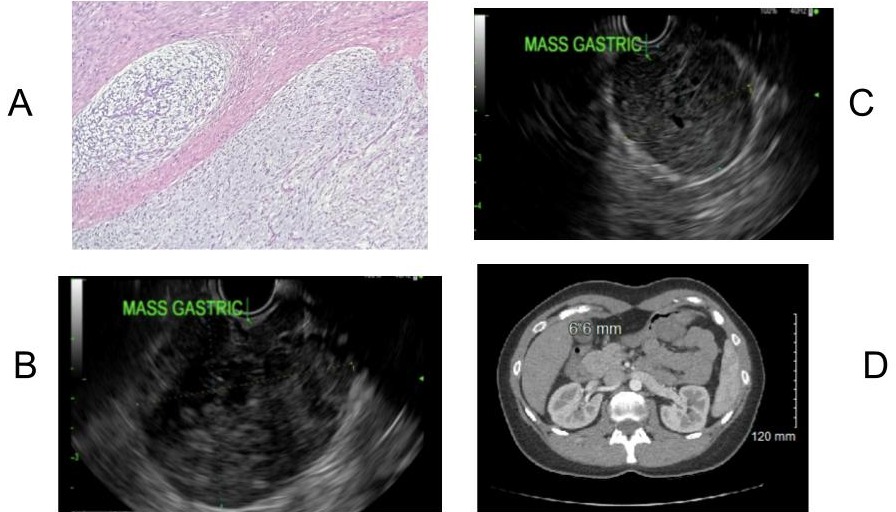
Figure: A) Sections show myxoid/fibro myxoid nodules with variable cellularity and spindle shaped lesional cells with bland cytologic features infiltrating through the muscularis and/or submucosal wall. There is no necrosis or increased mitotic activity seen. B) Endoscopic ultrasound of the PF. C) Endoscopic ultrasound of the PF. D) CT scan showing gastric mass.
Disclosures:
Megan Costello indicated no relevant financial relationships.
Lavina Thadani indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Erin Algeo indicated no relevant financial relationships.
Jason Singh indicated no relevant financial relationships.
John Campbell indicated no relevant financial relationships.
Megan Costello, BA1, Lavina Thadani, 1, Vinay Jahagirdar, MD1, Erin Algeo, DO1, Jason Singh, DO2, John Campbell, MD1. P5071 - Gastric Plexiform Fibromyxoma Associated With Secondary Hypertension: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

