Tuesday Poster Session
Category: Practice Management
P4896 - Rectal Examination Practices Amongst Gastroenterology Fellows and Advanced Practice Providers: A Quality Improvement Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rachel Thompson, MD
Yale New Haven Health
New Haven, CT
Presenting Author(s)
Rachel Thompson, MD1, Kyle Hickey, MD1, Jack Huebner, MD1, Rumzah Paracha, MD1, Amy Ogurick, MD2
1Yale New Haven Health, New Haven, CT; 2Yale Digestive Diseases and VA Connecticut Healthcare System, West Haven, CT
Introduction: Digital rectal examinations (DRE) are established as standard of care during initial evaluations for indications including constipation and dyssynergic defecation. Deficiencies in competence and confidence in DREs have been previously established, especially in trainees. Given the importance of DREs, our aim was to understand current DRE practices in gastroenterology (GI) clinic by fellows and advanced practice providers (APPs) to implement a quality improvement initiative for DRE standardization.
Methods: Gemba walk of an outpatient GI clinic was performed to identify initial process delays. A needs assessment survey was tested with a pilot group and then administered to current fellows and APPs in GI clinic. Survey questions were created using a 5-point Likert scale regarding frequency and confidence of performing DREs for various indications at an initial visit. Additional data was collected regarding documentation, chaperone accessibility, exam limitations, sensitive examination policies and anoscopy.
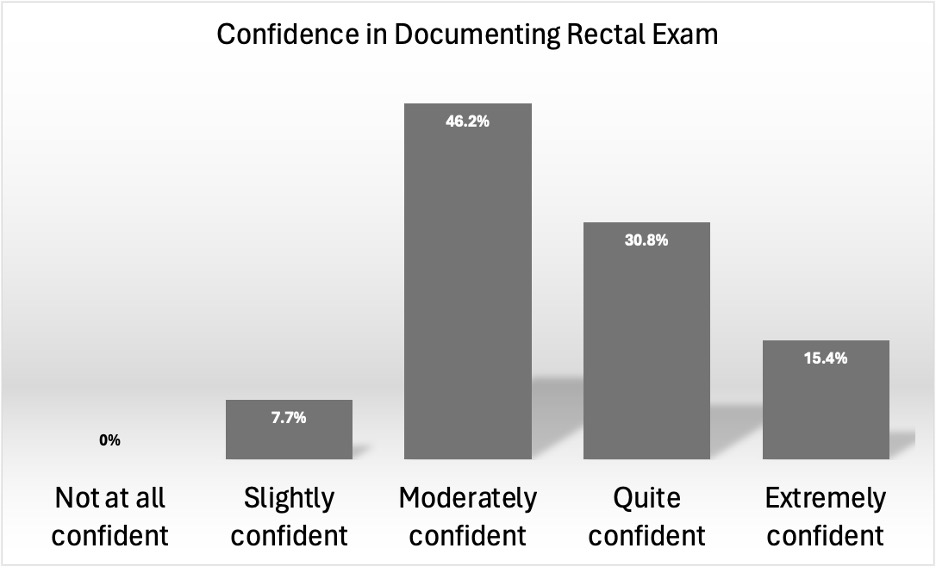
Results: 13 of 21 providers (10 fellows, 3 APPs responded, 62% response rate). Providers most consistently answered “almost always” to performing DREs for rectal bleeding and pain, less consistently for chronic constipation and fecal incontinence (Table 1). Providers were most confident in assessing for hemorrhoids, as opposed to anal fissures and dyssynergic defecation (Table 1) A large majority of respondents were not at all confident in performing anoscopy (Table 1). Most respondents were only slightly or moderately confident in documenting DREs (Figure 1). Limitations to performing DREs included time constraints (76.9%) and chaperone access (76.9%).
Discussion: DREs are not being consistently performed for initial encounters when they are clinically indicated. Providers have varied confidence in performing DREs across different exam indications. This study shows a discrepancy between providers’ perceived importance DREs by indication and performing them. There is also limited confidence in how to document a DRE. It has been previously established that structured educational interventions can significantly improve providers’ comfort and DRE skills. Next, we hope to review clinical encounters to determine frequency of DRE performance for indicated presentations and assess documentation quality. This will be followed by educational and clinic structural interventions to help overcome the barriers identified in this survey and standardize the practice of performing DREs in GI clinic.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rachel Thompson, MD1, Kyle Hickey, MD1, Jack Huebner, MD1, Rumzah Paracha, MD1, Amy Ogurick, MD2. P4896 - Rectal Examination Practices Amongst Gastroenterology Fellows and Advanced Practice Providers: A Quality Improvement Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale New Haven Health, New Haven, CT; 2Yale Digestive Diseases and VA Connecticut Healthcare System, West Haven, CT
Introduction: Digital rectal examinations (DRE) are established as standard of care during initial evaluations for indications including constipation and dyssynergic defecation. Deficiencies in competence and confidence in DREs have been previously established, especially in trainees. Given the importance of DREs, our aim was to understand current DRE practices in gastroenterology (GI) clinic by fellows and advanced practice providers (APPs) to implement a quality improvement initiative for DRE standardization.
Methods: Gemba walk of an outpatient GI clinic was performed to identify initial process delays. A needs assessment survey was tested with a pilot group and then administered to current fellows and APPs in GI clinic. Survey questions were created using a 5-point Likert scale regarding frequency and confidence of performing DREs for various indications at an initial visit. Additional data was collected regarding documentation, chaperone accessibility, exam limitations, sensitive examination policies and anoscopy.
Results: 13 of 21 providers (10 fellows, 3 APPs responded, 62% response rate). Providers most consistently answered “almost always” to performing DREs for rectal bleeding and pain, less consistently for chronic constipation and fecal incontinence (Table 1). Providers were most confident in assessing for hemorrhoids, as opposed to anal fissures and dyssynergic defecation (Table 1) A large majority of respondents were not at all confident in performing anoscopy (Table 1). Most respondents were only slightly or moderately confident in documenting DREs (Figure 1). Limitations to performing DREs included time constraints (76.9%) and chaperone access (76.9%).
Discussion: DREs are not being consistently performed for initial encounters when they are clinically indicated. Providers have varied confidence in performing DREs across different exam indications. This study shows a discrepancy between providers’ perceived importance DREs by indication and performing them. There is also limited confidence in how to document a DRE. It has been previously established that structured educational interventions can significantly improve providers’ comfort and DRE skills. Next, we hope to review clinical encounters to determine frequency of DRE performance for indicated presentations and assess documentation quality. This will be followed by educational and clinic structural interventions to help overcome the barriers identified in this survey and standardize the practice of performing DREs in GI clinic.
Figure: Confidence in rectal examinations varied across providers with 46.2% of respondents reporting feeling moderately confident
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rachel Thompson indicated no relevant financial relationships.
Kyle Hickey indicated no relevant financial relationships.
Jack Huebner indicated no relevant financial relationships.
Rumzah Paracha indicated no relevant financial relationships.
Amy Ogurick indicated no relevant financial relationships.
Rachel Thompson, MD1, Kyle Hickey, MD1, Jack Huebner, MD1, Rumzah Paracha, MD1, Amy Ogurick, MD2. P4896 - Rectal Examination Practices Amongst Gastroenterology Fellows and Advanced Practice Providers: A Quality Improvement Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

