Tuesday Poster Session
Category: Liver
P4811 - Hepatic Mycobacteroides abscessus Infection in an Immunocompetent Individual: A Case Report and Literature Review
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Zainab Mujahid, MD
University of Maryland Capital Region Health
Lorton, VA
Presenting Author(s)
Zainab Mujahid, MD1, Saeed Shoar, MD2, Mohammed Rifat Shaik, MBBS3, Eshan Nanda, MD4, Homayoon Mahjoob, MD, MPH5, Sunil Swami, MD2
1University of Maryland Capital Region Health, Lorton, VA; 2University of Maryland Capital Region Health, Largo, MD; 3University of Maryland Medical Center, Baltimore, MD; 4UPMC Harrisburg, Largo, PA; 5University of Maryland Capital Region Medical Center, Largo, MD
Introduction: Mycobacterium abscessus is the 2nd most common non-TB bacterial pathogen of the lung. Immunodeficient states such as HIV/AIDs, malignancy, and cirrhosis places individuals at increased risk for infection acquisition.Due to difficulty in organism isolation diagnosis is often delayed, compounding with multi-drug resistance leads to low cure rates.The atypical presentation as hepatic abscesses in our young healthy patient with was a notable diagnostic challenge.
Case Description/Methods: Jon Doe is a 21 yom with no PMH presenting with cough, intermittent fevers, night sweats, and progressive weight loss for the past two months. Vitals at presentation noted with BP 108/86, HR 110s, and temp 39.7 celsius. Physical exam demonstrated abdominal distension with diffuse tenderness without guarding or rigidity.
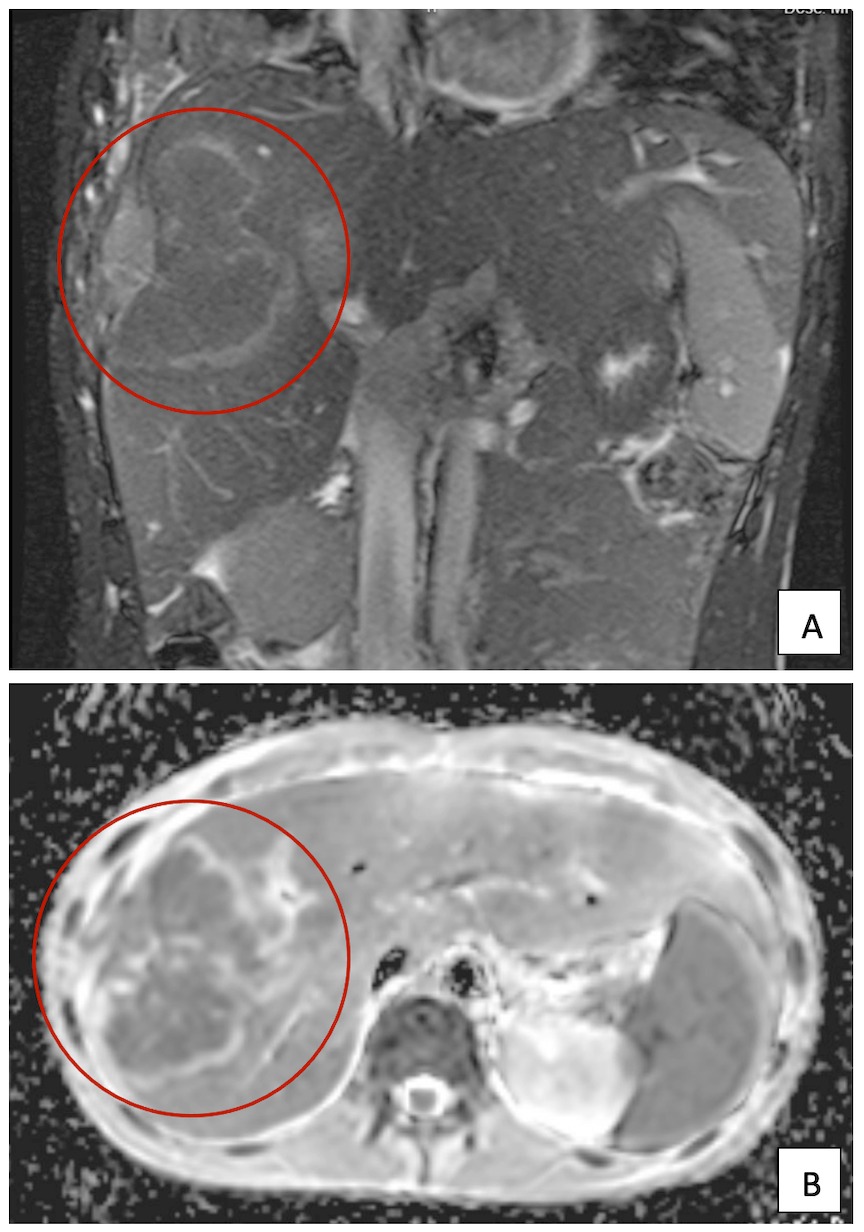
Infectious workup for HIV, CMV, EBV, VZV, TB, and hepatitis panel was negative.CT chest/abd/pelvis showed loculated effusion of the right lung with infiltrating mass extending into the right hepatic lobe, and multiple smaller masses in the left hepatic lobe.
Findings were concerning for a metastatic process however biopsy demonstrated PMN cells consistent with infection.Empiric antimicrobial with meropenem and albendazole was initiated, after two sets of fluid cultures was negative, with eventual third positive for M. Abscessus, the patient was transitioned to macrolide based tx and improved clinically.
Discussion: The most common organisms implicated in hepatic abscesses include staph a, strep, klebsiella, and e coli, however a broad differential is necessary due to emerging pathogens. M. Abscess due to its MDR and indolent course requires prolonged and aggressive abx regimen, often leaving patients at risk of under or delayed treatment.
Many subspecies of M. Abcessus are strict opportunistic pathogens. Of the reviewed case reports immunocompetent hosts presented with infection in the setting of indwelling foreign bodies.A study conducted by IDSA found 89% of M. Abscessus in non-HIV infected individuals had prior infection with opportunistic pathogens such as histoplasma, cryptococcus, and VZV suggesting prior immune cell reactivity may predispose to infection.
Our patient may be the first with this clinical picture lacking all the aforementioned risk factors.This may postulate initial empiric liver abscess treatment with macrolides in addition to usual penicillin/cephalosporin and metronidazole.Weighing risks and benefit as well as disease severity would ultimately guide treatment.
Disclosures:
Zainab Mujahid, MD1, Saeed Shoar, MD2, Mohammed Rifat Shaik, MBBS3, Eshan Nanda, MD4, Homayoon Mahjoob, MD, MPH5, Sunil Swami, MD2. P4811 - Hepatic Mycobacteroides abscessus Infection in an Immunocompetent Individual: A Case Report and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Capital Region Health, Lorton, VA; 2University of Maryland Capital Region Health, Largo, MD; 3University of Maryland Medical Center, Baltimore, MD; 4UPMC Harrisburg, Largo, PA; 5University of Maryland Capital Region Medical Center, Largo, MD
Introduction: Mycobacterium abscessus is the 2nd most common non-TB bacterial pathogen of the lung. Immunodeficient states such as HIV/AIDs, malignancy, and cirrhosis places individuals at increased risk for infection acquisition.Due to difficulty in organism isolation diagnosis is often delayed, compounding with multi-drug resistance leads to low cure rates.The atypical presentation as hepatic abscesses in our young healthy patient with was a notable diagnostic challenge.
Case Description/Methods: Jon Doe is a 21 yom with no PMH presenting with cough, intermittent fevers, night sweats, and progressive weight loss for the past two months. Vitals at presentation noted with BP 108/86, HR 110s, and temp 39.7 celsius. Physical exam demonstrated abdominal distension with diffuse tenderness without guarding or rigidity.
Infectious workup for HIV, CMV, EBV, VZV, TB, and hepatitis panel was negative.CT chest/abd/pelvis showed loculated effusion of the right lung with infiltrating mass extending into the right hepatic lobe, and multiple smaller masses in the left hepatic lobe.
Findings were concerning for a metastatic process however biopsy demonstrated PMN cells consistent with infection.Empiric antimicrobial with meropenem and albendazole was initiated, after two sets of fluid cultures was negative, with eventual third positive for M. Abscessus, the patient was transitioned to macrolide based tx and improved clinically.
Discussion: The most common organisms implicated in hepatic abscesses include staph a, strep, klebsiella, and e coli, however a broad differential is necessary due to emerging pathogens. M. Abscess due to its MDR and indolent course requires prolonged and aggressive abx regimen, often leaving patients at risk of under or delayed treatment.
Many subspecies of M. Abcessus are strict opportunistic pathogens. Of the reviewed case reports immunocompetent hosts presented with infection in the setting of indwelling foreign bodies.A study conducted by IDSA found 89% of M. Abscessus in non-HIV infected individuals had prior infection with opportunistic pathogens such as histoplasma, cryptococcus, and VZV suggesting prior immune cell reactivity may predispose to infection.
Our patient may be the first with this clinical picture lacking all the aforementioned risk factors.This may postulate initial empiric liver abscess treatment with macrolides in addition to usual penicillin/cephalosporin and metronidazole.Weighing risks and benefit as well as disease severity would ultimately guide treatment.
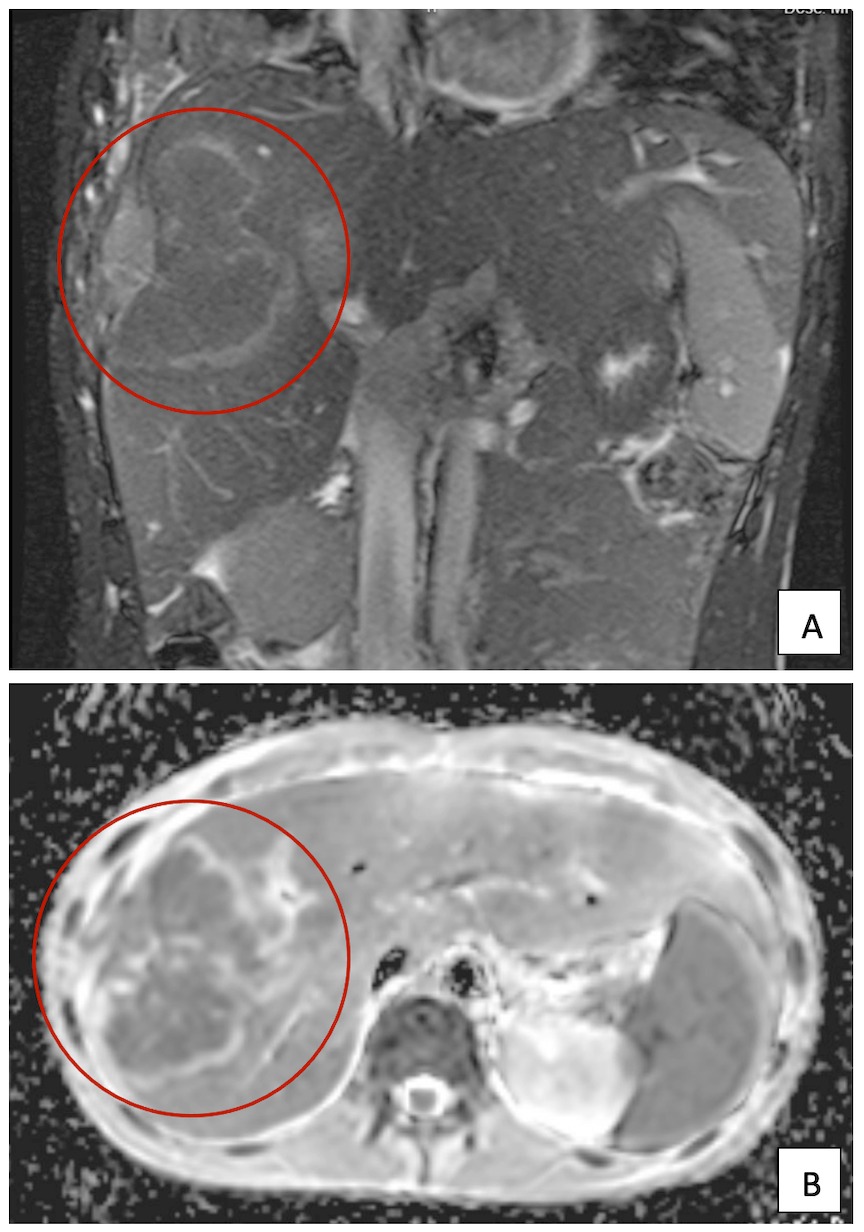
Figure: Contrast MRI: a) coronal section demonstrating 5.5cmx6.8cm abscess involving anatomic sections VII, VIII b) axial section involving lobes V, VI
Disclosures:
Zainab Mujahid indicated no relevant financial relationships.
Saeed Shoar indicated no relevant financial relationships.
Mohammed Rifat Shaik indicated no relevant financial relationships.
Eshan Nanda indicated no relevant financial relationships.
Homayoon Mahjoob indicated no relevant financial relationships.
Sunil Swami indicated no relevant financial relationships.
Zainab Mujahid, MD1, Saeed Shoar, MD2, Mohammed Rifat Shaik, MBBS3, Eshan Nanda, MD4, Homayoon Mahjoob, MD, MPH5, Sunil Swami, MD2. P4811 - Hepatic Mycobacteroides abscessus Infection in an Immunocompetent Individual: A Case Report and Literature Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
