Tuesday Poster Session
Category: Liver
P4813 - Lost in Compliance, Lost in Control: A Case of Wilson Disease and Neurological Decline
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MM
Miguel Martins, MD
Centro Hospitalar Universitário de São João
Porto, Porto, Portugal
Presenting Author(s)
Miguel Martins, MD1, Maria João. Almeida, MD1, Marina Magalhães, MD2, Susana Lopes, MD, PhD, FACG1, Guilherme Macedo, MD, PhD, FACG1
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2Santo Antonio University Hospital, Porto, Porto, Portugal
Introduction: This case underscores the importance of proper treatment and distinguishing MRI findings between Wilson’s disease and hepatocerebral degeneration.
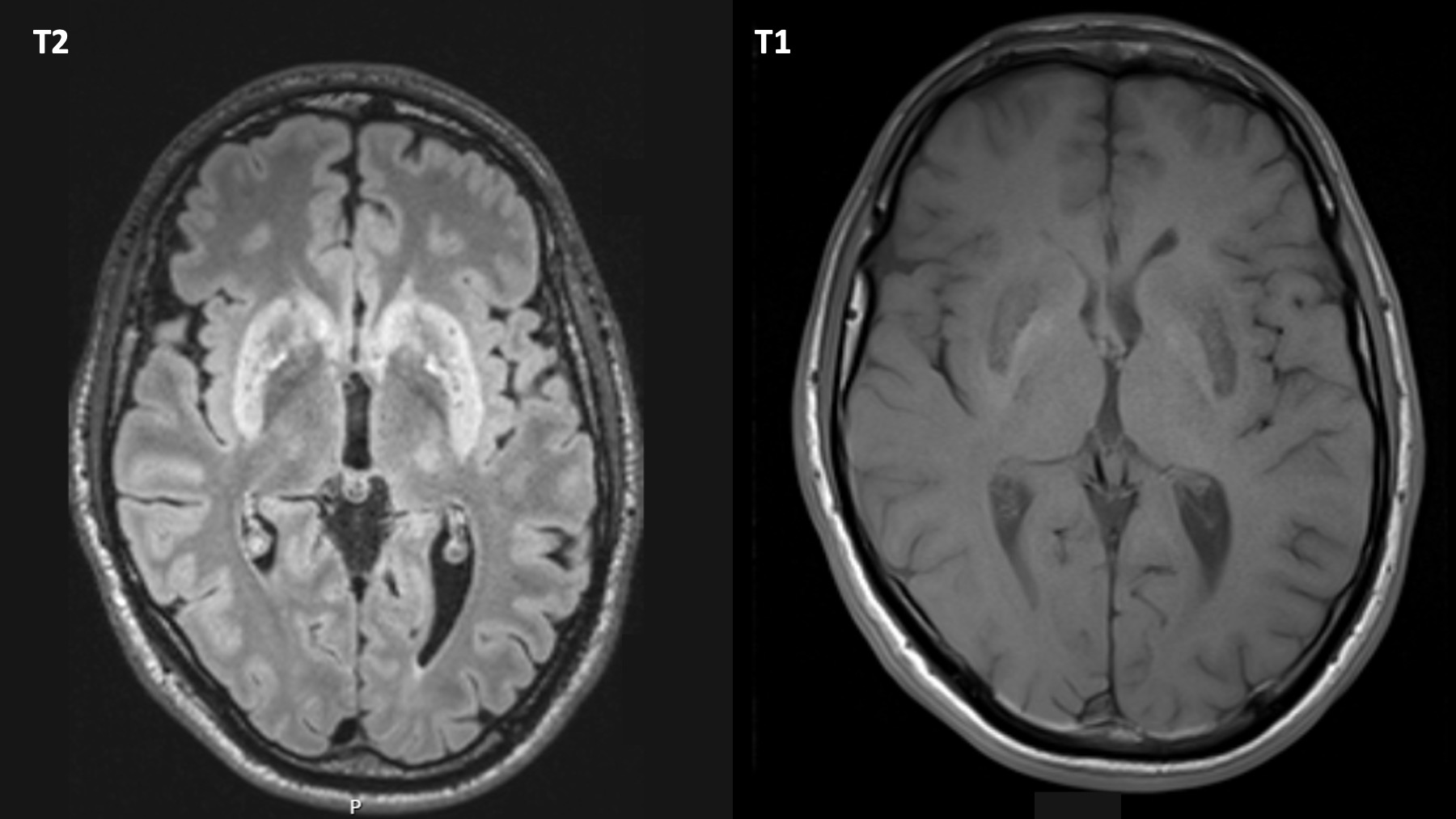
Case Description/Methods: A 29-year-old male diagnosed with Wilson disease at age 5 developed neuropsychiatric symptoms, tremor, and psychomotor slowing after non-adherence to copper chelation therapy. MRI revealed bilateral putaminal and caudate T2 hyperintensities extending to the protuberance and mesencephalon, along with T1 symmetric globus pallidus hyperintensity. Bilateral Kayser-Fleischer rings were present. Initial liver function tests were normal, and abdominal CT scans appeared unremarkable, but elastography and liver biopsy uncovered advanced fibrosis indicative of cirrhosis. Despite restarting chelation, a follow-up MRI after three months revealed persistent hyperintensities in the basal ganglia and pons.
Discussion: In Wilson’s disease, MRI typically shows hyperintensity in the basal ganglia and thalamus, with the rare occurrence of the "panda sign" in the midbrain. When neurological symptoms worsen, it can be challenging to determine if deterioration is due to increased brain copper or progression of cirrhosis leading to hepatocerebral degeneration. A classic indicator of hepatocerebral degeneration is T2 and T2 FLAIR hyperintensity in the middle cerebellar peduncles, with signal changes typically seen in T1, often more prominent in the globus pallidus and subthalamic nucleus. The hallmark of Wilson's disease, is putaminal T2 hyperintensity. The T1 signal in neuro-Wilson's disease varies depending on hepatic dysfunction.
Globus pallidus involvement raises the possibility of manganese accumulation, requiring further exploration. Traditional transplant criteria primarily consider liver function, but the patient's persistent neurological deterioration necessitates exploring liver transplantation as a potential intervention to address hepatocerebral degeneration. This case highlights the vital role of lifelong adherence to chelation therapy and vigilant monitoring for hepatic and neurological complications in Wilson disease. Transplantation has been successful in severe neurological impairment unresponsive to chelation therapy, indicating its potential as a valid option. Future research should investigate alternative risk stratification tools and long-term outcomes of liver transplantation in this specific population.
Disclosures:
Miguel Martins, MD1, Maria João. Almeida, MD1, Marina Magalhães, MD2, Susana Lopes, MD, PhD, FACG1, Guilherme Macedo, MD, PhD, FACG1. P4813 - Lost in Compliance, Lost in Control: A Case of Wilson Disease and Neurological Decline, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2Santo Antonio University Hospital, Porto, Porto, Portugal
Introduction: This case underscores the importance of proper treatment and distinguishing MRI findings between Wilson’s disease and hepatocerebral degeneration.
Case Description/Methods: A 29-year-old male diagnosed with Wilson disease at age 5 developed neuropsychiatric symptoms, tremor, and psychomotor slowing after non-adherence to copper chelation therapy. MRI revealed bilateral putaminal and caudate T2 hyperintensities extending to the protuberance and mesencephalon, along with T1 symmetric globus pallidus hyperintensity. Bilateral Kayser-Fleischer rings were present. Initial liver function tests were normal, and abdominal CT scans appeared unremarkable, but elastography and liver biopsy uncovered advanced fibrosis indicative of cirrhosis. Despite restarting chelation, a follow-up MRI after three months revealed persistent hyperintensities in the basal ganglia and pons.
Discussion: In Wilson’s disease, MRI typically shows hyperintensity in the basal ganglia and thalamus, with the rare occurrence of the "panda sign" in the midbrain. When neurological symptoms worsen, it can be challenging to determine if deterioration is due to increased brain copper or progression of cirrhosis leading to hepatocerebral degeneration. A classic indicator of hepatocerebral degeneration is T2 and T2 FLAIR hyperintensity in the middle cerebellar peduncles, with signal changes typically seen in T1, often more prominent in the globus pallidus and subthalamic nucleus. The hallmark of Wilson's disease, is putaminal T2 hyperintensity. The T1 signal in neuro-Wilson's disease varies depending on hepatic dysfunction.
Globus pallidus involvement raises the possibility of manganese accumulation, requiring further exploration. Traditional transplant criteria primarily consider liver function, but the patient's persistent neurological deterioration necessitates exploring liver transplantation as a potential intervention to address hepatocerebral degeneration. This case highlights the vital role of lifelong adherence to chelation therapy and vigilant monitoring for hepatic and neurological complications in Wilson disease. Transplantation has been successful in severe neurological impairment unresponsive to chelation therapy, indicating its potential as a valid option. Future research should investigate alternative risk stratification tools and long-term outcomes of liver transplantation in this specific population.
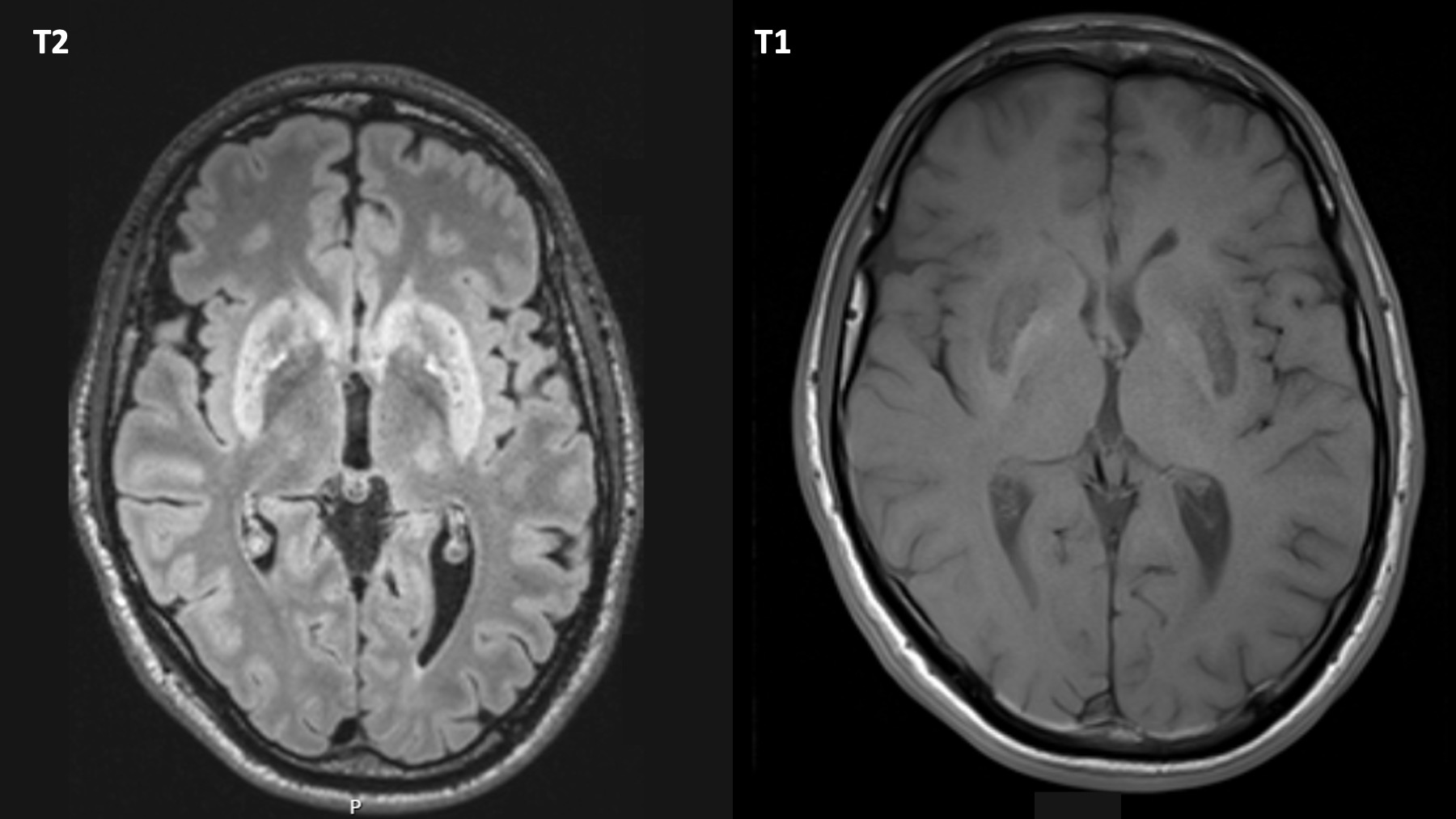
Figure: A 29-year-old male with Wilson disease developed neuropsychiatric symptoms after non-adherence to chelation therapy. MRI showed bilateral putaminal and caudate T2 and globus pallidus T1 hyperintensities.
Disclosures:
Miguel Martins indicated no relevant financial relationships.
Maria Almeida indicated no relevant financial relationships.
Marina Magalhães indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Miguel Martins, MD1, Maria João. Almeida, MD1, Marina Magalhães, MD2, Susana Lopes, MD, PhD, FACG1, Guilherme Macedo, MD, PhD, FACG1. P4813 - Lost in Compliance, Lost in Control: A Case of Wilson Disease and Neurological Decline, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
