Tuesday Poster Session
Category: Liver
P4815 - A Case of HBV Reactivation Causing Liver Deactivation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- MT
Manaswitha Thota, MD
Virginia Commonwealth University Medical Center
Richmond, VA
Presenting Author(s)
Manaswitha Thota, MD, Aldo Barajas-Ochoa, MD, Daniel Markley, DO, MPH
Virginia Commonwealth University Medical Center, Richmond, VA
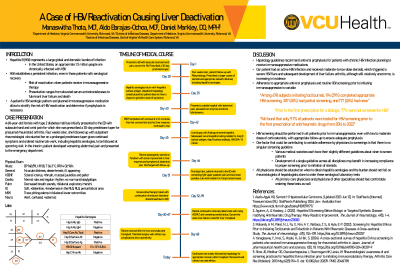
Introduction: Hepatitis B virus (HBV) establishes a persistent infection, even in patients with serological recovery. HBV can reactivate with immunosuppressive therapy, its presentation ranging from elevated serum aminotransferases to liver failure and death. It is critical to evaluate a patient’s HBV serologic status prior to initiating immunosuppression to stratify the risk of HBV reactivation and determine if prophylaxis is necessary. We present a case of severe HBV reactivation secondary to corticosteroid treatment of rheumatoid arthritis (RA), resulting in fulminant liver failure requiring transplant.
Case Description/Methods: A 68-year-old female with type 2 diabetes mellitus developed subacute hand arthritis, for which she was prescribed a 30-day prednisone taper (40mg for 4 days, 20mg for 4 days, 10mg for 22 days) and referred to rheumatology. Four weeks later, she was diagnosed with seropositive RA and prescribed hydroxychloroquine with prednisone taper (20mg daily for 3 weeks, 15 mg for 3 weeks, 10 mg for 3 weeks, and 5mg for 3 weeks). Laboratory testing showed normal transaminases, negative HBsAb, negative HBcAb-IgM, and positive HBsAg; no HBcAb-IgG or HBV DNA was obtained. A referral to hepatology was made. In the interim, steroids were continued and the patient was admitted for abdominal pain and elevated transaminases. Symptoms suspected to be due to obstructive jaundice and ERCP was completed with removal of a 5.6 cm stone. Despite removal, she continued to have rising transaminases. Liver biopsy showed severe hepatitis and HBV DNA PCR level was over 15 million IU/mL. She was started on tenofovir and discharged after stabilization of liver enzymes, but was re-admitted for worsening abdominal pain, developed grade 4 hepatic encephalopathy and fulminant liver failure with a MELD of 40, requiring liver transplant.
Discussion: Hepatology guidelines recommend antiviral prophylaxis for patients with chronic HBV infection planning to receive immunosuppressive medications. Our patient had an active HBV infection and received moderate-to-low dose steroids, which triggered a severe HBV flare and liver failure. Adherence to appropriate antiviral prophylaxis and routine HBV screening prior to initiating immunosuppression is variable, with some studies reporting HBV screening rates in patients with RA as low as 9.7%. HBV screening should be performed in all patients prior to immunosuppression, even with low to moderate doses of corticosteroids, with appropriate follow-up to ensure adequate prophylaxis.
Disclosures:
Manaswitha Thota, MD, Aldo Barajas-Ochoa, MD, Daniel Markley, DO, MPH. P4815 - A Case of HBV Reactivation Causing Liver Deactivation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Virginia Commonwealth University Medical Center, Richmond, VA
Introduction: Hepatitis B virus (HBV) establishes a persistent infection, even in patients with serological recovery. HBV can reactivate with immunosuppressive therapy, its presentation ranging from elevated serum aminotransferases to liver failure and death. It is critical to evaluate a patient’s HBV serologic status prior to initiating immunosuppression to stratify the risk of HBV reactivation and determine if prophylaxis is necessary. We present a case of severe HBV reactivation secondary to corticosteroid treatment of rheumatoid arthritis (RA), resulting in fulminant liver failure requiring transplant.
Case Description/Methods: A 68-year-old female with type 2 diabetes mellitus developed subacute hand arthritis, for which she was prescribed a 30-day prednisone taper (40mg for 4 days, 20mg for 4 days, 10mg for 22 days) and referred to rheumatology. Four weeks later, she was diagnosed with seropositive RA and prescribed hydroxychloroquine with prednisone taper (20mg daily for 3 weeks, 15 mg for 3 weeks, 10 mg for 3 weeks, and 5mg for 3 weeks). Laboratory testing showed normal transaminases, negative HBsAb, negative HBcAb-IgM, and positive HBsAg; no HBcAb-IgG or HBV DNA was obtained. A referral to hepatology was made. In the interim, steroids were continued and the patient was admitted for abdominal pain and elevated transaminases. Symptoms suspected to be due to obstructive jaundice and ERCP was completed with removal of a 5.6 cm stone. Despite removal, she continued to have rising transaminases. Liver biopsy showed severe hepatitis and HBV DNA PCR level was over 15 million IU/mL. She was started on tenofovir and discharged after stabilization of liver enzymes, but was re-admitted for worsening abdominal pain, developed grade 4 hepatic encephalopathy and fulminant liver failure with a MELD of 40, requiring liver transplant.
Discussion: Hepatology guidelines recommend antiviral prophylaxis for patients with chronic HBV infection planning to receive immunosuppressive medications. Our patient had an active HBV infection and received moderate-to-low dose steroids, which triggered a severe HBV flare and liver failure. Adherence to appropriate antiviral prophylaxis and routine HBV screening prior to initiating immunosuppression is variable, with some studies reporting HBV screening rates in patients with RA as low as 9.7%. HBV screening should be performed in all patients prior to immunosuppression, even with low to moderate doses of corticosteroids, with appropriate follow-up to ensure adequate prophylaxis.
Disclosures:
Manaswitha Thota indicated no relevant financial relationships.
Aldo Barajas-Ochoa indicated no relevant financial relationships.
Daniel Markley indicated no relevant financial relationships.
Manaswitha Thota, MD, Aldo Barajas-Ochoa, MD, Daniel Markley, DO, MPH. P4815 - A Case of HBV Reactivation Causing Liver Deactivation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
