Tuesday Poster Session
Category: Liver
P4749 - Hepatic Vein Thrombosis Secondary to an Entamoeba histolytica Infection
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Curtis Petruzzelli, MD
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Curtis Petruzzelli, MD, Tyler Selig, MD, Rachel Simmons, MD
Brown University / Rhode Island Hospital, Providence, RI
Introduction: Entamoeba histolytica is an intestinal protozoan that causes intestinal amebiasis and liver abscesses. In rarer instances, the hepatic abscesses formed by this parasite can be associated with venous thrombosis. Here we present a case of an older male who presented with subacute diarrhea and was found to have intestinal amebiasis along with liver abscesses complicated by hepatic vein thrombosis.
Case Description/Methods: A 69-year-old male with a history of distant tapeworm infection presented to the hospital for one month of diarrhea accompanied by generalized abdominal pain, nausea, and two days of fever, chills, night sweats, and confusion. Notably, a month prior to presentation he returned from 3-week trip to Panama. During this vacation, he swam in fecal-infested water and was exposed to unsanitary food. A week into his trip, the patient developed brown diarrhea with occasional red bloody streaks. Once he developed rigors, night sweats and confusion, he sought medical care.
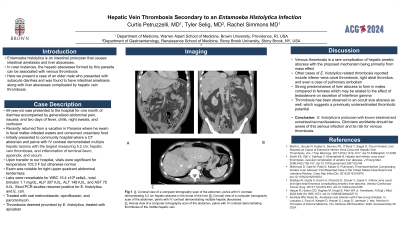
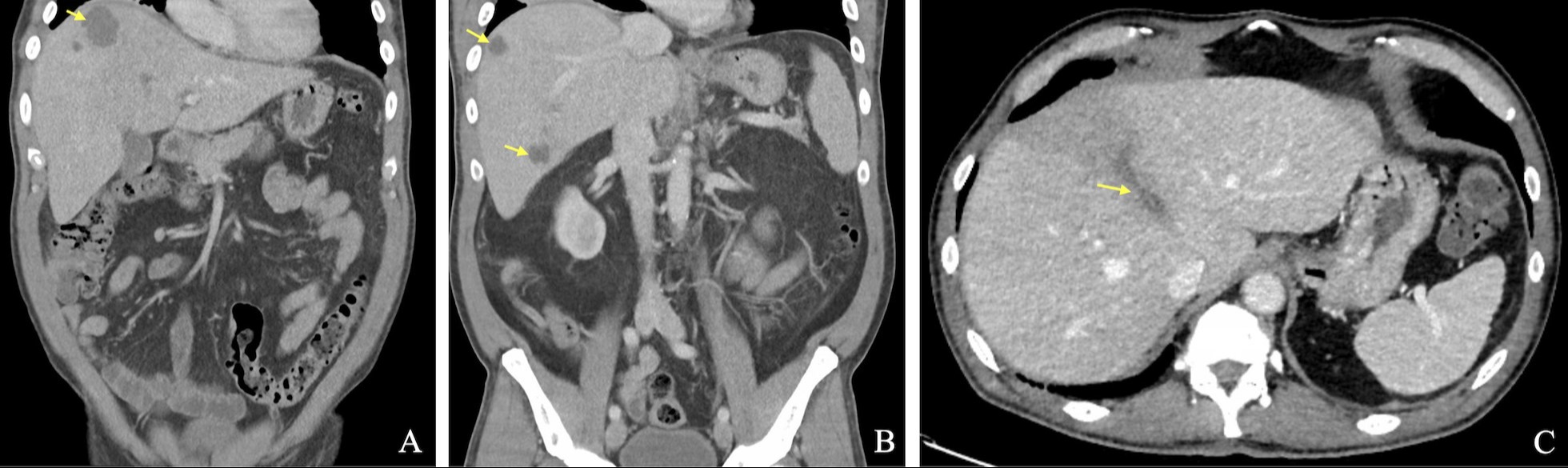
The patient was initially evaluated at a small community hospital where a CT abdomen and pelvis with IV contrast demonstrated multiple hepatic lesions with the largest measuring 5.2 cm, middle hepatic vein thrombosis, and inflammation of terminal ileum, appendix, and cecum (Figures A-C). Upon transfer to our tertiary hospital, vitals were significant for temperature 103.3 F but otherwise normal. Exam was notable for right upper quadrant abdominal tenderness. His labs were remarkable for WBC 15.4 x109 cells/L, total bilirubin 1.1 mg/dL, alkaline phosphatase 307 IU/L, ALT 148 IU/L, and AST 75 IU/L. Stool PCR studies returned positive for E. histolytica and E. coli. Percutaneous aspiration of a 2.2 cm hepatic abscess was performed but otherwise was medically managed with piperacillin-tazobactam and metronidazole before being transitioned to an oral metronidazole, ciprofloxacin, and paromomycin. The hepatic vein thrombus was deemed provoked by the infection per hematology and treated with apixaban. He was discharged on hospital day 5 in improved condition with outpatient follow up.
Discussion: Venous thrombosis is a rare complication of hepatic amebic abscess with the proposed mechanism being primarily from mass effect. However, thrombosis has been seen in an occult size abscess as well, which suggests a previously underestimated thrombotic potential of these abscesses. Clinicians worldwide should be aware of this serious infection and its risk for venous thrombosis.
Disclosures:
Curtis Petruzzelli, MD, Tyler Selig, MD, Rachel Simmons, MD. P4749 - Hepatic Vein Thrombosis Secondary to an Entamoeba histolytica Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Brown University / Rhode Island Hospital, Providence, RI
Introduction: Entamoeba histolytica is an intestinal protozoan that causes intestinal amebiasis and liver abscesses. In rarer instances, the hepatic abscesses formed by this parasite can be associated with venous thrombosis. Here we present a case of an older male who presented with subacute diarrhea and was found to have intestinal amebiasis along with liver abscesses complicated by hepatic vein thrombosis.
Case Description/Methods: A 69-year-old male with a history of distant tapeworm infection presented to the hospital for one month of diarrhea accompanied by generalized abdominal pain, nausea, and two days of fever, chills, night sweats, and confusion. Notably, a month prior to presentation he returned from 3-week trip to Panama. During this vacation, he swam in fecal-infested water and was exposed to unsanitary food. A week into his trip, the patient developed brown diarrhea with occasional red bloody streaks. Once he developed rigors, night sweats and confusion, he sought medical care.
The patient was initially evaluated at a small community hospital where a CT abdomen and pelvis with IV contrast demonstrated multiple hepatic lesions with the largest measuring 5.2 cm, middle hepatic vein thrombosis, and inflammation of terminal ileum, appendix, and cecum (Figures A-C). Upon transfer to our tertiary hospital, vitals were significant for temperature 103.3 F but otherwise normal. Exam was notable for right upper quadrant abdominal tenderness. His labs were remarkable for WBC 15.4 x109 cells/L, total bilirubin 1.1 mg/dL, alkaline phosphatase 307 IU/L, ALT 148 IU/L, and AST 75 IU/L. Stool PCR studies returned positive for E. histolytica and E. coli. Percutaneous aspiration of a 2.2 cm hepatic abscess was performed but otherwise was medically managed with piperacillin-tazobactam and metronidazole before being transitioned to an oral metronidazole, ciprofloxacin, and paromomycin. The hepatic vein thrombus was deemed provoked by the infection per hematology and treated with apixaban. He was discharged on hospital day 5 in improved condition with outpatient follow up.
Discussion: Venous thrombosis is a rare complication of hepatic amebic abscess with the proposed mechanism being primarily from mass effect. However, thrombosis has been seen in an occult size abscess as well, which suggests a previously underestimated thrombotic potential of these abscesses. Clinicians worldwide should be aware of this serious infection and its risk for venous thrombosis.
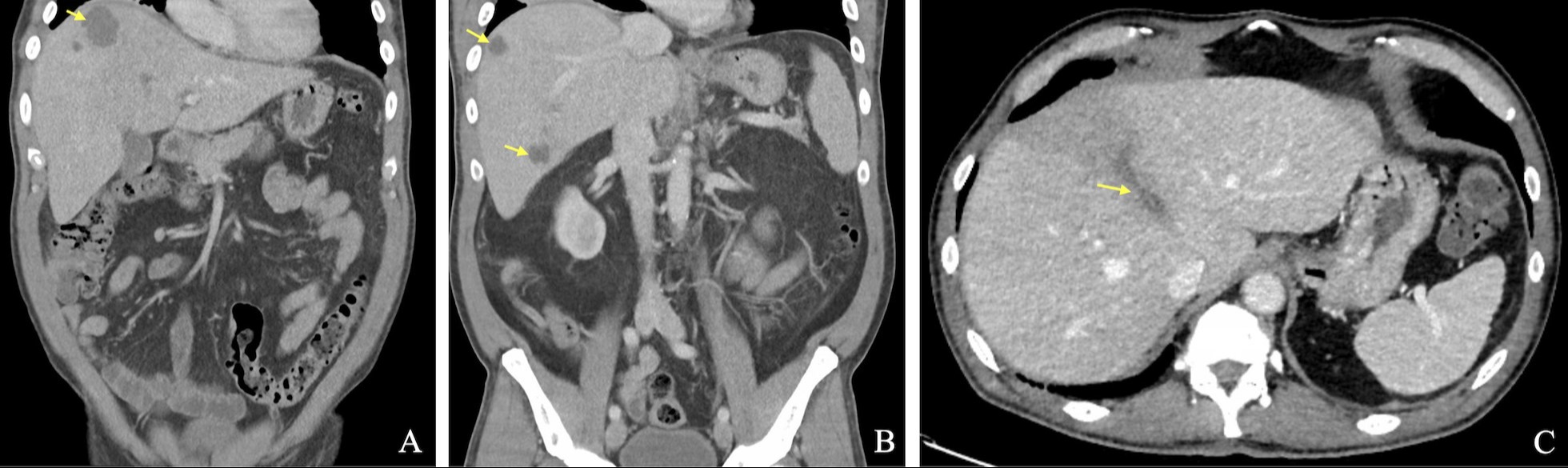
Figure: Figure A. Coronal view of a CT scan of the abdomen/pelvis with IV contrast demonstrating a 5.2 cm hepatic abscess in the dome of the liver.
Figure B. Coronal view of a CT scan of the abdomen/pelvis with IV contrast demonstrating multiple hepatic abscesses.
Figure C. Axonal view of a CT scan of the abdomen/pelvis with IV contrast demonstrating the middle hepatic vein thrombus.
Figure B. Coronal view of a CT scan of the abdomen/pelvis with IV contrast demonstrating multiple hepatic abscesses.
Figure C. Axonal view of a CT scan of the abdomen/pelvis with IV contrast demonstrating the middle hepatic vein thrombus.
Disclosures:
Curtis Petruzzelli indicated no relevant financial relationships.
Tyler Selig indicated no relevant financial relationships.
Rachel Simmons indicated no relevant financial relationships.
Curtis Petruzzelli, MD, Tyler Selig, MD, Rachel Simmons, MD. P4749 - Hepatic Vein Thrombosis Secondary to an Entamoeba histolytica Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
