Tuesday Poster Session
Category: Liver
P4761 - Salivary Gland Tumor Presenting as a Large Metastatic Hepatic Mass: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- IB
Ivan Berezowski, MD
George Washington University School of Medicine and Health Sciences
Washington, DC
Presenting Author(s)
Ivan Berezowski, MD1, Matthew Walker, BA1, Alisa Dewald, BS1, Reid Schalet, DO1, Jacob Newman, DO1, Mamoun Younes, MD2, Ameer Abutaleb, MD2, Zahid Vahora, MD2, Stephen Gray, MD2
1George Washington University School of Medicine and Health Sciences, Washington, DC; 2George Washington University Hospital, Washington, DC
Introduction: Salivary gland tumors are rare, representing 6-8% of head and neck tumors. Adenoid cystic carcinoma (ACC) and basal cell adenocarcinoma (BCAC) are two malignant subsets. ACCs represent 10% of salivary gland tumors and have high rates of metastasis. BCACs account for < 1%, are locally destructive and rarely metastasize. We herein report the case of a patient with a metastatic salivary gland tumor who presented with a significant hepatic mass initially believed to be a primary tumor.
Case Description/Methods: A 29-year-old male presented to the emergency department (ED) for right upper quadrant pain and early satiety. A computed tomography (CT) scan revealed hepatomegaly with a 14cm left hepatic mass. He was discharged with outpatient hepatology follow-up. He returned one month later with the same symptoms, and magnetic resonance imaging (MRI) showed a 19cm enhancing hepatic mass. After appropriate pain control, he was discharged. The patient was lost to follow-up, presenting to a different ED the following month for abdominal pain, early satiety, and unintentional 10lb weight loss. MRI revealed a 21.5cm enhancing hepatic mass and, with concern for hepatocellular carcinoma, he was admitted for biopsy and staging. Laboratory workup was unrevealing. CT revealed innumerable bilateral pulmonary nodules. Preliminary pathology review of biopsy revealed a well-differentiated carcinoma with myxoid stroma. The patient underwent transcatheter arterial chemoembolization (TACE) and was discharged with oncology follow-up. Two weeks later he underwent TACE again, as well as biopsy of a newly noted right parotid mass. On both biopsies, immunohistochemistry favored ACC, however BCAC could not be excluded. A diagnosis was made of stage IV adenoid cystic carcinoma with metastases to liver and lung. Given tremendous tumor burden and poor prognosis, treatment goals became palliative, and the patient was started on cisplatin and vinorelbine.
Discussion: We report a case of a patient with metastatic salivary gland tumor who presented with a significant hepatic mass initially believed to be a primary tumor. Metastatic salivary gland tumors are rare, with only four previous accounts in the literature. Treatment modalities for these cases are poorly understood due to their rarity, as well as high degree of resistance to chemotherapeutic agents and recurrence following resection. Therefore, it is important to consider these patients on a case by case basis and discuss palliative treatment options to maximize comfort.
Disclosures:
Ivan Berezowski, MD1, Matthew Walker, BA1, Alisa Dewald, BS1, Reid Schalet, DO1, Jacob Newman, DO1, Mamoun Younes, MD2, Ameer Abutaleb, MD2, Zahid Vahora, MD2, Stephen Gray, MD2. P4761 - Salivary Gland Tumor Presenting as a Large Metastatic Hepatic Mass: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1George Washington University School of Medicine and Health Sciences, Washington, DC; 2George Washington University Hospital, Washington, DC
Introduction: Salivary gland tumors are rare, representing 6-8% of head and neck tumors. Adenoid cystic carcinoma (ACC) and basal cell adenocarcinoma (BCAC) are two malignant subsets. ACCs represent 10% of salivary gland tumors and have high rates of metastasis. BCACs account for < 1%, are locally destructive and rarely metastasize. We herein report the case of a patient with a metastatic salivary gland tumor who presented with a significant hepatic mass initially believed to be a primary tumor.
Case Description/Methods: A 29-year-old male presented to the emergency department (ED) for right upper quadrant pain and early satiety. A computed tomography (CT) scan revealed hepatomegaly with a 14cm left hepatic mass. He was discharged with outpatient hepatology follow-up. He returned one month later with the same symptoms, and magnetic resonance imaging (MRI) showed a 19cm enhancing hepatic mass. After appropriate pain control, he was discharged. The patient was lost to follow-up, presenting to a different ED the following month for abdominal pain, early satiety, and unintentional 10lb weight loss. MRI revealed a 21.5cm enhancing hepatic mass and, with concern for hepatocellular carcinoma, he was admitted for biopsy and staging. Laboratory workup was unrevealing. CT revealed innumerable bilateral pulmonary nodules. Preliminary pathology review of biopsy revealed a well-differentiated carcinoma with myxoid stroma. The patient underwent transcatheter arterial chemoembolization (TACE) and was discharged with oncology follow-up. Two weeks later he underwent TACE again, as well as biopsy of a newly noted right parotid mass. On both biopsies, immunohistochemistry favored ACC, however BCAC could not be excluded. A diagnosis was made of stage IV adenoid cystic carcinoma with metastases to liver and lung. Given tremendous tumor burden and poor prognosis, treatment goals became palliative, and the patient was started on cisplatin and vinorelbine.
Discussion: We report a case of a patient with metastatic salivary gland tumor who presented with a significant hepatic mass initially believed to be a primary tumor. Metastatic salivary gland tumors are rare, with only four previous accounts in the literature. Treatment modalities for these cases are poorly understood due to their rarity, as well as high degree of resistance to chemotherapeutic agents and recurrence following resection. Therefore, it is important to consider these patients on a case by case basis and discuss palliative treatment options to maximize comfort.
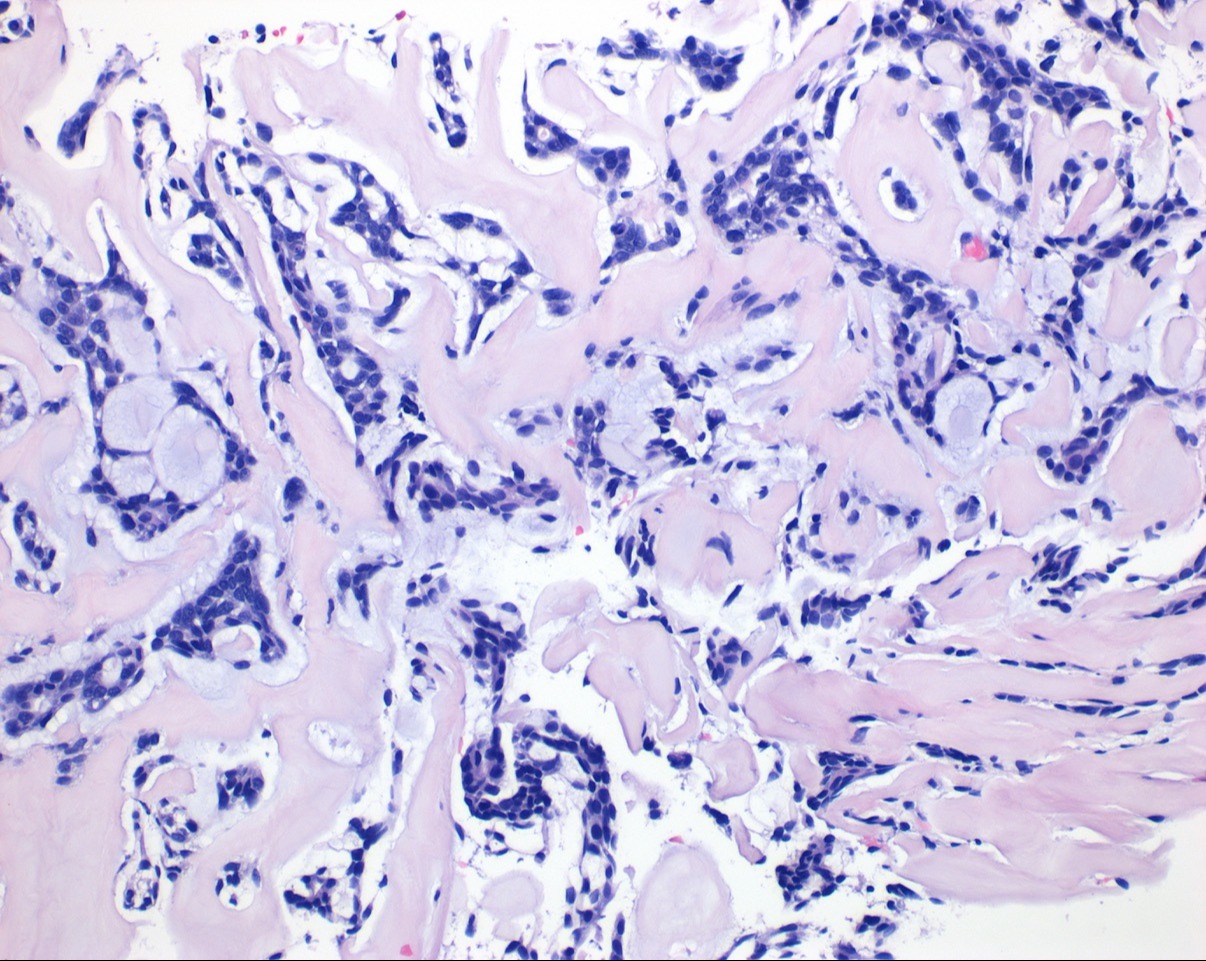
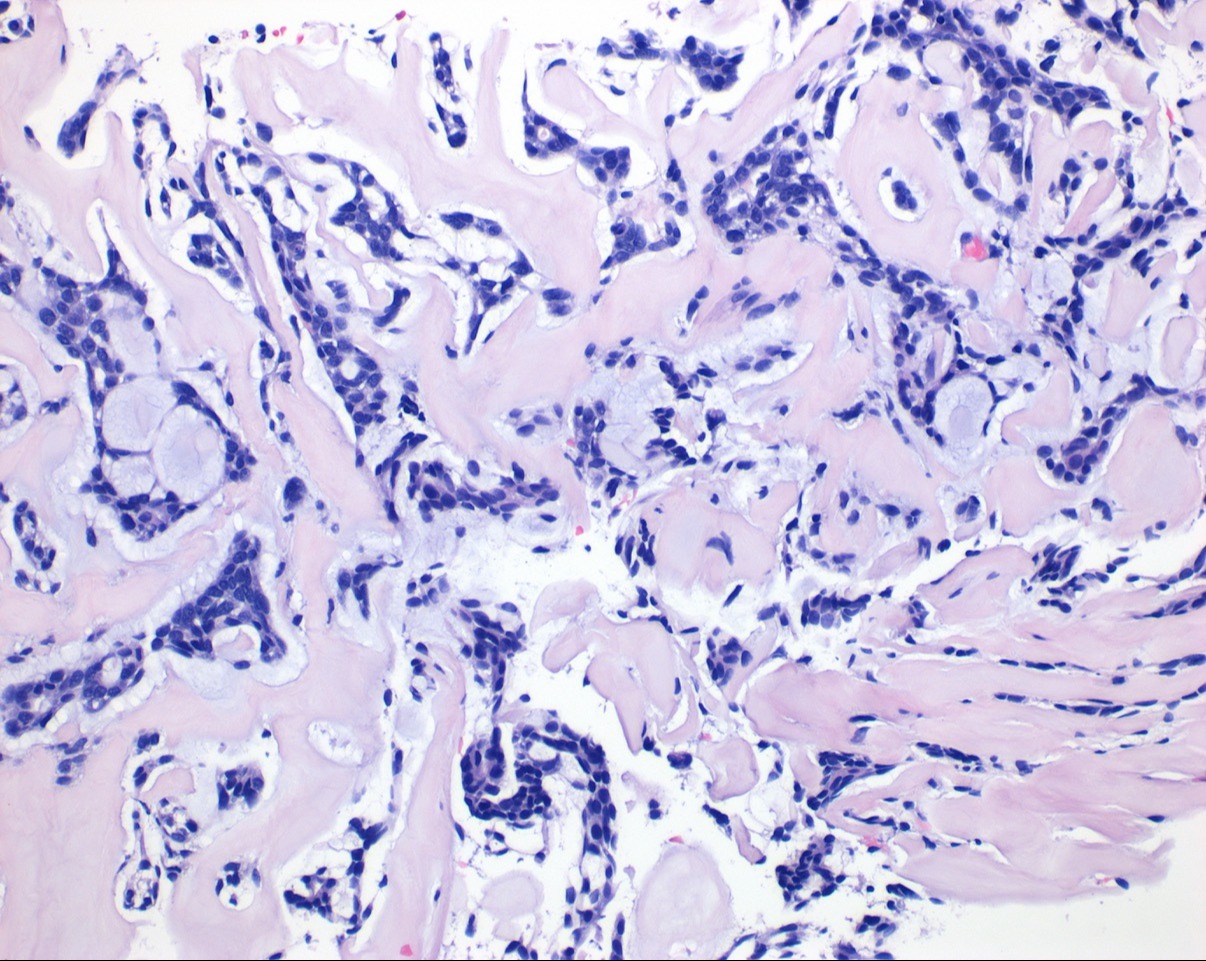
Figure: Microscopic appearance of the salivary gland showing tubular and cribriform structures in mucinous background (hematoxylin-eosin, × 20). Immunoperoxidase staining shows a dual cell population with the majority of cells positive for CK7 and a lesser population of cells positive for S100 and p63.
Disclosures:
Ivan Berezowski indicated no relevant financial relationships.
Matthew Walker indicated no relevant financial relationships.
Alisa Dewald indicated no relevant financial relationships.
Reid Schalet indicated no relevant financial relationships.
Jacob Newman indicated no relevant financial relationships.
Mamoun Younes indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Zahid Vahora: Abbvie – Speakers Bureau.
Stephen Gray indicated no relevant financial relationships.
Ivan Berezowski, MD1, Matthew Walker, BA1, Alisa Dewald, BS1, Reid Schalet, DO1, Jacob Newman, DO1, Mamoun Younes, MD2, Ameer Abutaleb, MD2, Zahid Vahora, MD2, Stephen Gray, MD2. P4761 - Salivary Gland Tumor Presenting as a Large Metastatic Hepatic Mass: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
