Tuesday Poster Session
Category: Liver
P4673 - Cirrhotic Patients Admitted With ST-Segment Elevation Myocardial Infarction Undergo Less Percutaneous Coronary Intervention and Experience Higher Mortality Rates: A Nationwide Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

M Kenan Rahima, MD
TriHealth Good Samaritan Hospital
Cincinnati, OH
Presenting Author(s)
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Bassel Bitar, MD1, Tarek Aboursheid, MD3, Venkata Muddana, MD4
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3Ascension Saint Francis Hospital, Evanston, IL; 4TriHealth, Cincinnati, OH
Introduction: The decision to perform percutaneous coronary intervention (PCI) in cirrhotic patients presenting with ST-segment elevation myocardial infarction (STEMI) is challenging. While PCI is the standard of care for STEMI and can significantly improve outcomes, the procedure carries higher risks for patients with cirrhosis. The literature suggests that the proportion of cirrhotic patients undergoing PCI varies widely, reflecting the complexity and risks associated with these interventions in this population and there is limited scientific evidence examining outcomes in this population. Thus, our objective was to assess clinical outcomes in this specific population.
Methods: We accessed the National Inpatient Sample from 2017-2020 to identify adult patients with cirrhosis hospitalized due to STEMI and the proportion of those who undergo PCI. We further analyzed the cirrhotic & STEMI cohort with PCI vs non-PCI group. pro The primary endpoint was inpatient mortality, with secondary endpoints including cardiac arrest, gastrointestinal bleeding (GIB), intubation, length of stay (LOS), and total hospital charges. We utilized multivariable logistic regression analysis to estimate clinical outcomes, with a significance threshold of P < 0.05.
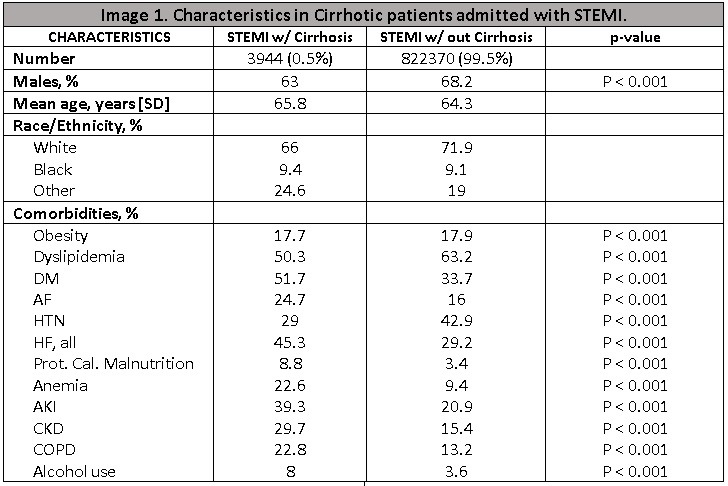
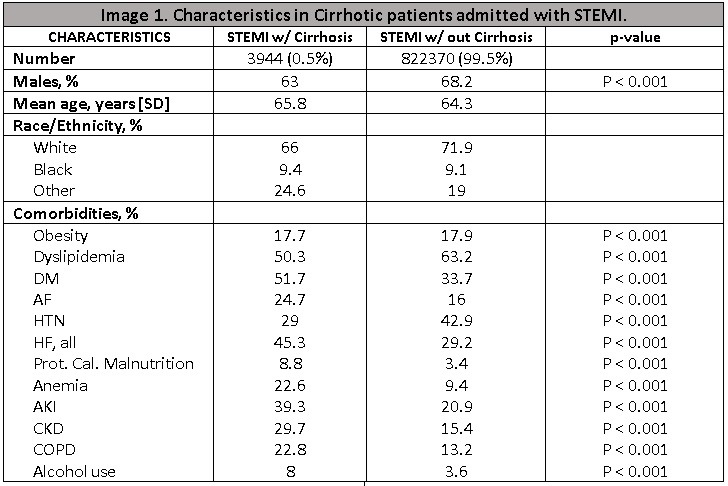
Results: We identified 826,315 hospitalizations with STEMI, among which 3,944 (0.4%) presented with cirrhosis. Comparing cirrhotic and non-cirrhotic cohorts shows almost the same age and gender rates with statistically significant variation in comorbidities that are present in Image 1. Clinical outcomes revealed stark differences where the cirrhotic cohort had a higher mortality rate with an odds ratio (OR) of 1.67 (CI 1.34 –2) and underwent less PCI with an OR of 0.68 (CI 0.57-0.81). We further compared cirrhotic patients with STEMI who received and who didn’t receive PCI. We identified that 49.4% of cirrhotic patients with STEMI had PCI and had lower statistically significant mortality with OR of 0.28[0.18-0.44] and better clinical outcomes in Table 1. All data were adjusted for various factors including age, sex, race, comorbidity indices, obesity, Afib, DM, HTN, PVD, AKI, CKD, nicotine and alcohol use, stroke, acute respiratory failure, and inflation during 2017-2020.
Discussion: We concluded that patients with cirrhosis who had STEMI tend to have higher mortality and undergo less PCI compared to those who don’t have cirrhosis. Moreover, we found that almost half of the cirrhotic patients with STEMI get PCI which is associated with better clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Bassel Bitar, MD1, Tarek Aboursheid, MD3, Venkata Muddana, MD4. P4673 - Cirrhotic Patients Admitted With ST-Segment Elevation Myocardial Infarction Undergo Less Percutaneous Coronary Intervention and Experience Higher Mortality Rates: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3Ascension Saint Francis Hospital, Evanston, IL; 4TriHealth, Cincinnati, OH
Introduction: The decision to perform percutaneous coronary intervention (PCI) in cirrhotic patients presenting with ST-segment elevation myocardial infarction (STEMI) is challenging. While PCI is the standard of care for STEMI and can significantly improve outcomes, the procedure carries higher risks for patients with cirrhosis. The literature suggests that the proportion of cirrhotic patients undergoing PCI varies widely, reflecting the complexity and risks associated with these interventions in this population and there is limited scientific evidence examining outcomes in this population. Thus, our objective was to assess clinical outcomes in this specific population.
Methods: We accessed the National Inpatient Sample from 2017-2020 to identify adult patients with cirrhosis hospitalized due to STEMI and the proportion of those who undergo PCI. We further analyzed the cirrhotic & STEMI cohort with PCI vs non-PCI group. pro The primary endpoint was inpatient mortality, with secondary endpoints including cardiac arrest, gastrointestinal bleeding (GIB), intubation, length of stay (LOS), and total hospital charges. We utilized multivariable logistic regression analysis to estimate clinical outcomes, with a significance threshold of P < 0.05.
Results: We identified 826,315 hospitalizations with STEMI, among which 3,944 (0.4%) presented with cirrhosis. Comparing cirrhotic and non-cirrhotic cohorts shows almost the same age and gender rates with statistically significant variation in comorbidities that are present in Image 1. Clinical outcomes revealed stark differences where the cirrhotic cohort had a higher mortality rate with an odds ratio (OR) of 1.67 (CI 1.34 –2) and underwent less PCI with an OR of 0.68 (CI 0.57-0.81). We further compared cirrhotic patients with STEMI who received and who didn’t receive PCI. We identified that 49.4% of cirrhotic patients with STEMI had PCI and had lower statistically significant mortality with OR of 0.28[0.18-0.44] and better clinical outcomes in Table 1. All data were adjusted for various factors including age, sex, race, comorbidity indices, obesity, Afib, DM, HTN, PVD, AKI, CKD, nicotine and alcohol use, stroke, acute respiratory failure, and inflation during 2017-2020.
Discussion: We concluded that patients with cirrhosis who had STEMI tend to have higher mortality and undergo less PCI compared to those who don’t have cirrhosis. Moreover, we found that almost half of the cirrhotic patients with STEMI get PCI which is associated with better clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Kenan Rahima indicated no relevant financial relationships.
Mohamad Hijazi indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bassel Bitar indicated no relevant financial relationships.
Tarek Aboursheid indicated no relevant financial relationships.
Venkata Muddana indicated no relevant financial relationships.
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Bassel Bitar, MD1, Tarek Aboursheid, MD3, Venkata Muddana, MD4. P4673 - Cirrhotic Patients Admitted With ST-Segment Elevation Myocardial Infarction Undergo Less Percutaneous Coronary Intervention and Experience Higher Mortality Rates: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
