Tuesday Poster Session
Category: Liver
P4678 - Gap in Care: Follow-Up of Incidental Hepatic Steatosis on Imaging in a Urban Safety Net Hospital
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- VS
Venkata Sunkesula, MD, MS
MetroHealth Medical Center
Cleveland, OH
Presenting Author(s)
Venkata Sunkesula, MD, MS1, Rishi Chowdhary, MD2, Isaac Dahan, MD1, Richard Blinkhorn, MD1, Ronnie Fass, MD3, Bolin Niu, MD3
1MetroHealth Medical Center, Cleveland, OH; 2Metrohealth Medical Center, Cleveland, OH; 3Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Nonalcoholic fatty liver disease (NAFLD) results from fat accumulation in the liver without heavy alcohol use or other causes. Patients often receive the diagnosis after steatosis is identified on imaging ordered by primary care physicians (PCP) and emergency department (ED) providers. Since clear guidelines for managing this incidental finding are lacking, our objective is to determine the level of follow up patients received as a result of this finding. We hypothesize that incidental steatosis on imaging would not be addressed in a majority of patients.
Methods: We identified 241 patients with incidental hepatic steatosis in 2019 and 2020 at The MetroHealth System in Cleveland, OH, by reviewing imaging studies obtained in outpatient (OP) and emergency room (ED) settings. Radiology reports with incidental steatosis were identified using keywords “steatosis” or “fatty liver”. Abdominal ultrasound (US), MRI, and CT abdomen were included. We excluded patients with history of drug, alcohol abuse, fatty liver, cirrhosis, viral hepatitis, and primary liver diseases. Through chart review we determined if a hepatology referral, fibroscan, or liver function test was ordered within 12 months of the incidental finding. Patient characteristics, and co-morbidities were compared between the ED and OP encounters. Data were analyzed with GraphPad.
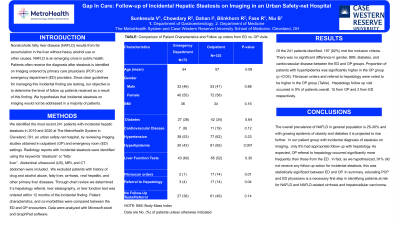
Results: Of 241 patients identified, 197 (82%) met inclusion criteria. There was no significant difference in gender, BMI, diabetes, and cardiovascular disease between ED and OP groups. Proportion of patients with hyperlipidemia was significantly higher in the OP group (p < 0.05). Fibroscan orders and referral to hepatology were higher in the OP group (Table). Hepatology follow up visit occurred in 9% of patients, 15 from OP and 3 from ED respectively.
Discussion: The overall prevalence of NAFLD in general population is 25-30% and with growing epidemic of obesity and diabetes it is projected to rise further. In our patient group with incidental diagnosis of steatosis on imaging, only 9% had appropriate follow up with hepatology. As expected, OP referral to hepatology occurred significantly more frequently than those from the ED. In fact, as we hypothesized, 91% did not receive any follow up action for incidental steatosis, this was statistically significant between ED and OP. In summary, educating PCP and ED physicians is a necessary first step in identifying patients at risk for NAFLD and NAFLD-related cirrhosis and hepatocellular carcinoma.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Venkata Sunkesula, MD, MS1, Rishi Chowdhary, MD2, Isaac Dahan, MD1, Richard Blinkhorn, MD1, Ronnie Fass, MD3, Bolin Niu, MD3. P4678 - Gap in Care: Follow-Up of Incidental Hepatic Steatosis on Imaging in a Urban Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MetroHealth Medical Center, Cleveland, OH; 2Metrohealth Medical Center, Cleveland, OH; 3Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Nonalcoholic fatty liver disease (NAFLD) results from fat accumulation in the liver without heavy alcohol use or other causes. Patients often receive the diagnosis after steatosis is identified on imaging ordered by primary care physicians (PCP) and emergency department (ED) providers. Since clear guidelines for managing this incidental finding are lacking, our objective is to determine the level of follow up patients received as a result of this finding. We hypothesize that incidental steatosis on imaging would not be addressed in a majority of patients.
Methods: We identified 241 patients with incidental hepatic steatosis in 2019 and 2020 at The MetroHealth System in Cleveland, OH, by reviewing imaging studies obtained in outpatient (OP) and emergency room (ED) settings. Radiology reports with incidental steatosis were identified using keywords “steatosis” or “fatty liver”. Abdominal ultrasound (US), MRI, and CT abdomen were included. We excluded patients with history of drug, alcohol abuse, fatty liver, cirrhosis, viral hepatitis, and primary liver diseases. Through chart review we determined if a hepatology referral, fibroscan, or liver function test was ordered within 12 months of the incidental finding. Patient characteristics, and co-morbidities were compared between the ED and OP encounters. Data were analyzed with GraphPad.
Results: Of 241 patients identified, 197 (82%) met inclusion criteria. There was no significant difference in gender, BMI, diabetes, and cardiovascular disease between ED and OP groups. Proportion of patients with hyperlipidemia was significantly higher in the OP group (p < 0.05). Fibroscan orders and referral to hepatology were higher in the OP group (Table). Hepatology follow up visit occurred in 9% of patients, 15 from OP and 3 from ED respectively.
Discussion: The overall prevalence of NAFLD in general population is 25-30% and with growing epidemic of obesity and diabetes it is projected to rise further. In our patient group with incidental diagnosis of steatosis on imaging, only 9% had appropriate follow up with hepatology. As expected, OP referral to hepatology occurred significantly more frequently than those from the ED. In fact, as we hypothesized, 91% did not receive any follow up action for incidental steatosis, this was statistically significant between ED and OP. In summary, educating PCP and ED physicians is a necessary first step in identifying patients at risk for NAFLD and NAFLD-related cirrhosis and hepatocellular carcinoma.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Venkata Sunkesula indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Isaac Dahan indicated no relevant financial relationships.
Richard Blinkhorn indicated no relevant financial relationships.
Ronnie Fass indicated no relevant financial relationships.
Bolin Niu indicated no relevant financial relationships.
Venkata Sunkesula, MD, MS1, Rishi Chowdhary, MD2, Isaac Dahan, MD1, Richard Blinkhorn, MD1, Ronnie Fass, MD3, Bolin Niu, MD3. P4678 - Gap in Care: Follow-Up of Incidental Hepatic Steatosis on Imaging in a Urban Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
