Tuesday Poster Session
Category: Interventional Endoscopy
P4509 - ERCP, Stent, and Beyond: A Rare Sequence of Events Post-Cholecystectomy Leading to Pneumoperitoneum
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sandeep Gill, BS
Midwestern University Arizona College of Osteopathic Medicine
Tustin, CA
Presenting Author(s)
Award: Presidential Poster Award
Sandeep Gill, BS1, Faisal Mehmood, MD2, Hajra Jamil, MD3, Joseph Fares, MD4, Gavin Levinthal, MD4
1Midwestern University Arizona College of Osteopathic Medicine, Tustin, CA; 2HonorHealth, Phoenix, AZ; 3Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 4HonorHealth, Scottsdale, AZ
Introduction: Pneumoperitoneum after abdominal surgery is a confounding finding with uncertain significance. A diagnostic perplexity often arises. It can represent residual postoperative pneumoperitoneum, which will need no intervention, or a complication such as a perforation of the gastrointestinal tract surgical intervention.
Case Description/Methods: A 64-year-old female presented to the emergency room for intermittent epigastric pain for 2 weeks. The pain was radiating to the right upper quadrant, aggravated by meals and alleviated by taking Tums. She had associated subjective fevers, chills, and bilious emesis. She denies using any alcohol or smoking cigarettes.
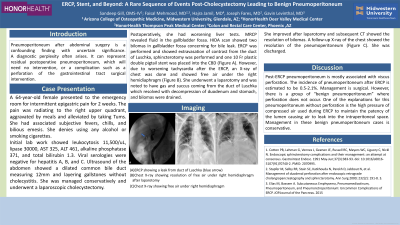
Initial lab work showed leukocytosis 11,500/uL, lipase 30000, AST 325, ALT 461, alkaline phosphatase 371, and total bilirubin 1.3. Viral serologies were negative for hepatitis A, B, and C. Ultrasound of the abdomen showed a dilated common bile duct measuring 12mm and layering gallstones without cholecystitis. She was managed conservatively and underwent a laparoscopic cholecystectomy. Postoperatively, she had worsening liver tests. MRCP revealed fluid in the gallbladder fossa. HIDA scan showed two bilomas in gallbladder fossa concerning for bile leak. ERCP was performed and showed extravasation of contrast from the duct of Luschka, sphincterotomy was performed and one 10 Fr plastic double pigtail stent was placed into the common bile duct (Figure A). However, due to worsening tachycardia after the ERCP, an X-ray of chest was done and showed free air under the right hemidiaphragm (Figure B). She underwent a laparotomy and was noted to have gas and succus coming from the duct of Luschka which resolved with decompression of duodenum and stomach, and bilomas were drained. The patient improved clinically after laparotomy and subsequent CT showed the resolution of bilomas. A follow-up X-ray of the chest showed the resolution of the pneumoperitoneum (Figure C). She was discharged in a stable condition.
Discussion: Post-ERCP pneumoperitoneum is mostly associated with viscus perforation. The incidence of pneumoperitoneum after ERCP is estimated to be 0.5-2.1%. Management is surgical. However, there is a group of “benign pneumoperitoneum” where perforation does not occur. One of the explanations for this pneumoperitoneum without perforation is the high pressure of compressed air used during ERCP to maintain the patency of the lumen causing air to leak into the intraperitoneal space. Management in these benign pneumoperitoneum cases is conservative.

Disclosures:
Sandeep Gill, BS1, Faisal Mehmood, MD2, Hajra Jamil, MD3, Joseph Fares, MD4, Gavin Levinthal, MD4. P4509 - ERCP, Stent, and Beyond: A Rare Sequence of Events Post-Cholecystectomy Leading to Pneumoperitoneum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Sandeep Gill, BS1, Faisal Mehmood, MD2, Hajra Jamil, MD3, Joseph Fares, MD4, Gavin Levinthal, MD4
1Midwestern University Arizona College of Osteopathic Medicine, Tustin, CA; 2HonorHealth, Phoenix, AZ; 3Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 4HonorHealth, Scottsdale, AZ
Introduction: Pneumoperitoneum after abdominal surgery is a confounding finding with uncertain significance. A diagnostic perplexity often arises. It can represent residual postoperative pneumoperitoneum, which will need no intervention, or a complication such as a perforation of the gastrointestinal tract surgical intervention.
Case Description/Methods: A 64-year-old female presented to the emergency room for intermittent epigastric pain for 2 weeks. The pain was radiating to the right upper quadrant, aggravated by meals and alleviated by taking Tums. She had associated subjective fevers, chills, and bilious emesis. She denies using any alcohol or smoking cigarettes.
Initial lab work showed leukocytosis 11,500/uL, lipase 30000, AST 325, ALT 461, alkaline phosphatase 371, and total bilirubin 1.3. Viral serologies were negative for hepatitis A, B, and C. Ultrasound of the abdomen showed a dilated common bile duct measuring 12mm and layering gallstones without cholecystitis. She was managed conservatively and underwent a laparoscopic cholecystectomy. Postoperatively, she had worsening liver tests. MRCP revealed fluid in the gallbladder fossa. HIDA scan showed two bilomas in gallbladder fossa concerning for bile leak. ERCP was performed and showed extravasation of contrast from the duct of Luschka, sphincterotomy was performed and one 10 Fr plastic double pigtail stent was placed into the common bile duct (Figure A). However, due to worsening tachycardia after the ERCP, an X-ray of chest was done and showed free air under the right hemidiaphragm (Figure B). She underwent a laparotomy and was noted to have gas and succus coming from the duct of Luschka which resolved with decompression of duodenum and stomach, and bilomas were drained. The patient improved clinically after laparotomy and subsequent CT showed the resolution of bilomas. A follow-up X-ray of the chest showed the resolution of the pneumoperitoneum (Figure C). She was discharged in a stable condition.
Discussion: Post-ERCP pneumoperitoneum is mostly associated with viscus perforation. The incidence of pneumoperitoneum after ERCP is estimated to be 0.5-2.1%. Management is surgical. However, there is a group of “benign pneumoperitoneum” where perforation does not occur. One of the explanations for this pneumoperitoneum without perforation is the high pressure of compressed air used during ERCP to maintain the patency of the lumen causing air to leak into the intraperitoneal space. Management in these benign pneumoperitoneum cases is conservative.

Figure: (A) ERCP showing a leak from duct of Luschka (blue arrow)
(B) Chest X-ray showing free air under right hemidiaphragm
(C) Chest X-ray showing resolution of free air under right hemidiaphragm after laparotomy
(B) Chest X-ray showing free air under right hemidiaphragm
(C) Chest X-ray showing resolution of free air under right hemidiaphragm after laparotomy
Disclosures:
Sandeep Gill indicated no relevant financial relationships.
Faisal Mehmood indicated no relevant financial relationships.
Hajra Jamil indicated no relevant financial relationships.
Joseph Fares indicated no relevant financial relationships.
Gavin Levinthal indicated no relevant financial relationships.
Sandeep Gill, BS1, Faisal Mehmood, MD2, Hajra Jamil, MD3, Joseph Fares, MD4, Gavin Levinthal, MD4. P4509 - ERCP, Stent, and Beyond: A Rare Sequence of Events Post-Cholecystectomy Leading to Pneumoperitoneum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

