Tuesday Poster Session
Category: IBD
P4427 - The Brain and The Gut: Often Overlooked Connections in Inflammatory Bowel Disease and Parkinson’s Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Stephanie Saey, MD
Mayo Clinic School of Graduate Medical Education
Rochester, MN
Presenting Author(s)
Stephanie Saey, MD1, Natalie Griffin, MD2, Adam Bledsoe, MD2
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2Mayo Clinic, Rochester, MN
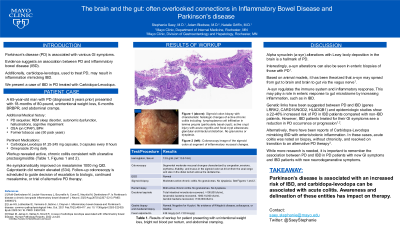
Introduction: Parkinson’s disease (PD) is associated with various GI symptoms. Evidence suggests association between PD and inflammatory bowel disease (IBD). Additionally, carbidopa-levodopa, used to treat PD, may result in inflammation mimicking IBD. We present a case of IBD in PD treated with carbidopa-levodopa.
Case Description/Methods: A 65-year-old man with PD on carbidopa/levodopa presented with 18-months of 80-pound, unintentional weight loss, 6-months of bright red blood per rectum, and abdominal cramping. Fecal calprotectin was elevated at 439. Colonoscopy showed moderate inflammation continuously from the rectum through the sigmoid colon, characterized by congestion, erosions, erythema, friability and mucus. There was the suggestion of a cecal patch. Biopsies showed active, chronic colitis consistent with ulcerative proctosigmoiditis. The patient was initiated on mesalamine 1000mg QID and symptomatically improved. However, calprotectin remained elevated. Follow up colonoscopy is scheduled to guide the decision of escalation to biologic, continued mesalamine, or trial of alternative PD therapy.
Discussion: Alpha synuclein (a-syn) alterations with Lewy body deposition in the brain is a hallmark of PD. Interestingly, a-syn alterations can also be seen in enteric biopsies of those with PD. Based on animal models, it has been theorized that a-syn may spread from gut to brain and brain to gut via the vagus nerve. A-syn regulates the immune system and inflammatory response. This may play a role in enteric response to gut microbiome by increasing inflammation, such as in IBD. Genetic links have been suggested between PD and IBD (genes LRRK2, CARD15/NOD2, and HLADQB1) and epidemiologic studies show a 22-46% increased risk of PD in IBD patients compared with non-IBD patients. However, IBD patients treated for their GI symptoms see a reduction in PD occurrence or progression. Alternatively, there have been reports of Carbidopa-Levodopa mimicking IBD with enteric/colonic inflammation. In these cases, acute colitis was noted on biopsy, without chronicity, and resolved on transition to an alternative PD therapy. While more research is needed, it is important to remember the association between PD and IBD in PD patients with new GI symptoms and IBD patients with new neurodegenerative symptoms. Clinicians should consider carbidopa-levodopa may cause acute colitis in a PD patient.
Disclosures:
Stephanie Saey, MD1, Natalie Griffin, MD2, Adam Bledsoe, MD2. P4427 - The Brain and The Gut: Often Overlooked Connections in Inflammatory Bowel Disease and Parkinson’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2Mayo Clinic, Rochester, MN
Introduction: Parkinson’s disease (PD) is associated with various GI symptoms. Evidence suggests association between PD and inflammatory bowel disease (IBD). Additionally, carbidopa-levodopa, used to treat PD, may result in inflammation mimicking IBD. We present a case of IBD in PD treated with carbidopa-levodopa.
Case Description/Methods: A 65-year-old man with PD on carbidopa/levodopa presented with 18-months of 80-pound, unintentional weight loss, 6-months of bright red blood per rectum, and abdominal cramping. Fecal calprotectin was elevated at 439. Colonoscopy showed moderate inflammation continuously from the rectum through the sigmoid colon, characterized by congestion, erosions, erythema, friability and mucus. There was the suggestion of a cecal patch. Biopsies showed active, chronic colitis consistent with ulcerative proctosigmoiditis. The patient was initiated on mesalamine 1000mg QID and symptomatically improved. However, calprotectin remained elevated. Follow up colonoscopy is scheduled to guide the decision of escalation to biologic, continued mesalamine, or trial of alternative PD therapy.
Discussion: Alpha synuclein (a-syn) alterations with Lewy body deposition in the brain is a hallmark of PD. Interestingly, a-syn alterations can also be seen in enteric biopsies of those with PD. Based on animal models, it has been theorized that a-syn may spread from gut to brain and brain to gut via the vagus nerve. A-syn regulates the immune system and inflammatory response. This may play a role in enteric response to gut microbiome by increasing inflammation, such as in IBD. Genetic links have been suggested between PD and IBD (genes LRRK2, CARD15/NOD2, and HLADQB1) and epidemiologic studies show a 22-46% increased risk of PD in IBD patients compared with non-IBD patients. However, IBD patients treated for their GI symptoms see a reduction in PD occurrence or progression. Alternatively, there have been reports of Carbidopa-Levodopa mimicking IBD with enteric/colonic inflammation. In these cases, acute colitis was noted on biopsy, without chronicity, and resolved on transition to an alternative PD therapy. While more research is needed, it is important to remember the association between PD and IBD in PD patients with new GI symptoms and IBD patients with new neurodegenerative symptoms. Clinicians should consider carbidopa-levodopa may cause acute colitis in a PD patient.
Disclosures:
Stephanie Saey indicated no relevant financial relationships.
Natalie Griffin indicated no relevant financial relationships.
Adam Bledsoe: Chugai Pharma – Grant/Research Support. Kanyos Bio – Grant/Research Support.
Stephanie Saey, MD1, Natalie Griffin, MD2, Adam Bledsoe, MD2. P4427 - The Brain and The Gut: Often Overlooked Connections in Inflammatory Bowel Disease and Parkinson’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
