Tuesday Poster Session
Category: IBD
P4430 - Dysplasia Surveillance in PSC-IBD; A Case For Concern
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mary Sullivan, MD
University of Virginia
Charlottesville, VA
Presenting Author(s)
Mary Sullivan, MD1, Gianna Stoleru, MD2, Esteban Figueroa, MD1
1University of Virginia, Charlottesville, VA; 2University of Virginia Medical Center, Charlottesville, VA
Introduction: Patients with primary sclerosing cholangitis (PSC) have a high degree of association with inflammatory bowel disease (IBD). Although patients with PSC often have mild to asymptomatic IBD, they are at increased risk for colitis associated cancer (CAC) and should undergo annual endoscopic surveillance for detection of dysplasia.
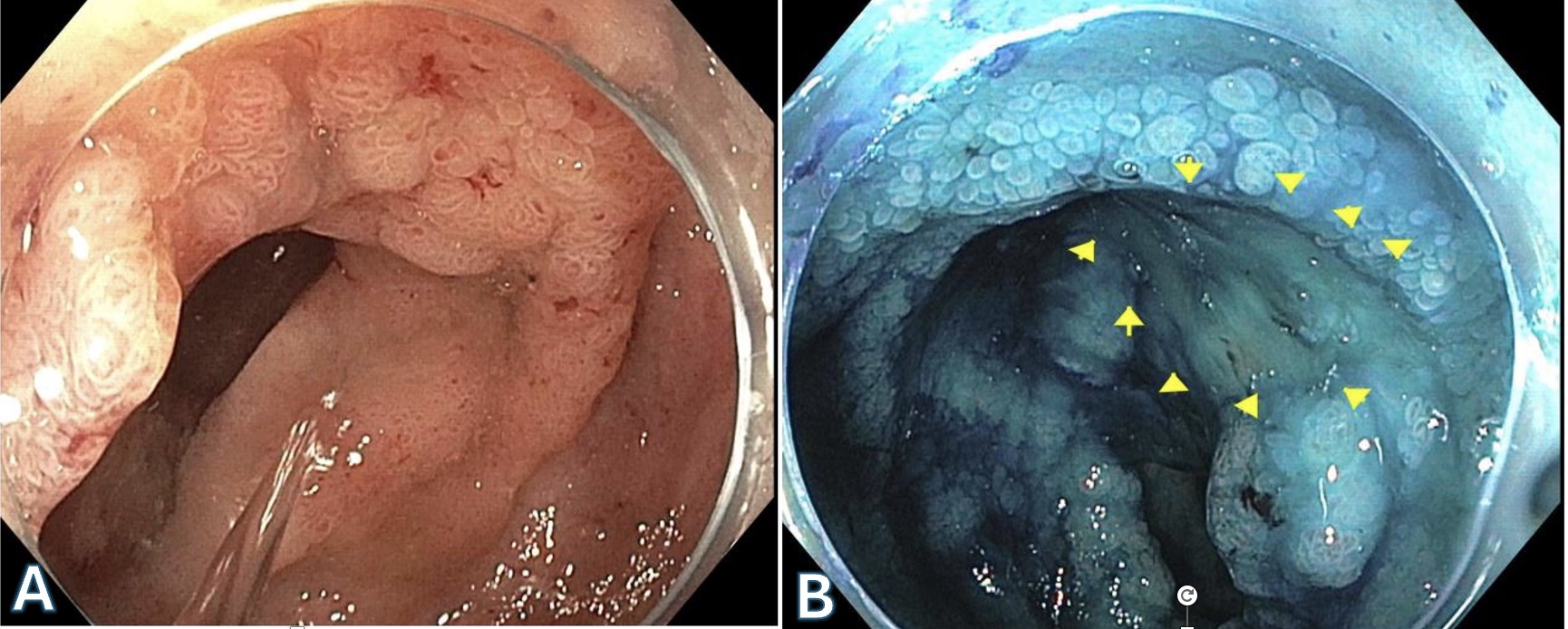
Case Description/Methods: This case presents a 53-year-old female with no past medical history who presented to an outside clinic for years of diarrhea and weight loss. She was found to have UC (Ulcerative Colitis) and an area of endoscopically visible lesion which resulted as low-grade dysplasia at the hepatic flexure on initial diagnostic colonoscopy. Subsequently, due to abnormal LFTs, she underwent an MRI which showed intrahepatic biliary ductal dilation with stricturing consistent with PSC. She was referred to our clinic for dye spray chromoendoscopy for further characterization of her dysplastic lesion, which resulted as Mayo Score 1 inflammation from the rectum to cecum and a 30 mm polypoid lesion at the hepatic flexure that was classified as NICE Type III on NBI. After dye spray chromoendoscopy with methylene blue the lesion had indistinct borders, loss of mucosal surface pattern and an area of central depression. Biopsies were taken which revealed invasive adenocarcinoma. The patient was referred to surgery for total colectomy but opted for a right hemicolectomy. On her surgically resected pathology specimen there was another synchronous cancer found. She underwent surveillance colonoscopy at 5 months postoperatively which was notable for a non-polypoid lesion characterized by a localized area of granular mucosa in the rectosigmoid. Examination with NBI demonstrated distinct borders but complete loss of mucosal surface pattern. Biopsies showed well differentiated adenocarcinoma and she underwent completion proctocolectomy. However, two lymph nodes demonstrated metastatic adenocarcinoma.
Discussion: Patients with PSC-IBD are at a higher risk of developing CRC despite having minimal or even quiescent inflammatory disease. This case emphasizes the importance of endoscopic surveillance for dysplasia as well as utilization of dye spray chromoendoscopy in order to accurately characterize concerning lesions. Despite limited evidence in PSC-IBD, current best practice is to undergo dysplasia surveillance at time of diagnosis and annually thereafter. Patients with PSC-IBD are at increased risk of synchronous cancer and treatment decisions should take this into account.
Disclosures:
Mary Sullivan, MD1, Gianna Stoleru, MD2, Esteban Figueroa, MD1. P4430 - Dysplasia Surveillance in PSC-IBD; A Case For Concern, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Virginia, Charlottesville, VA; 2University of Virginia Medical Center, Charlottesville, VA
Introduction: Patients with primary sclerosing cholangitis (PSC) have a high degree of association with inflammatory bowel disease (IBD). Although patients with PSC often have mild to asymptomatic IBD, they are at increased risk for colitis associated cancer (CAC) and should undergo annual endoscopic surveillance for detection of dysplasia.
Case Description/Methods: This case presents a 53-year-old female with no past medical history who presented to an outside clinic for years of diarrhea and weight loss. She was found to have UC (Ulcerative Colitis) and an area of endoscopically visible lesion which resulted as low-grade dysplasia at the hepatic flexure on initial diagnostic colonoscopy. Subsequently, due to abnormal LFTs, she underwent an MRI which showed intrahepatic biliary ductal dilation with stricturing consistent with PSC. She was referred to our clinic for dye spray chromoendoscopy for further characterization of her dysplastic lesion, which resulted as Mayo Score 1 inflammation from the rectum to cecum and a 30 mm polypoid lesion at the hepatic flexure that was classified as NICE Type III on NBI. After dye spray chromoendoscopy with methylene blue the lesion had indistinct borders, loss of mucosal surface pattern and an area of central depression. Biopsies were taken which revealed invasive adenocarcinoma. The patient was referred to surgery for total colectomy but opted for a right hemicolectomy. On her surgically resected pathology specimen there was another synchronous cancer found. She underwent surveillance colonoscopy at 5 months postoperatively which was notable for a non-polypoid lesion characterized by a localized area of granular mucosa in the rectosigmoid. Examination with NBI demonstrated distinct borders but complete loss of mucosal surface pattern. Biopsies showed well differentiated adenocarcinoma and she underwent completion proctocolectomy. However, two lymph nodes demonstrated metastatic adenocarcinoma.
Discussion: Patients with PSC-IBD are at a higher risk of developing CRC despite having minimal or even quiescent inflammatory disease. This case emphasizes the importance of endoscopic surveillance for dysplasia as well as utilization of dye spray chromoendoscopy in order to accurately characterize concerning lesions. Despite limited evidence in PSC-IBD, current best practice is to undergo dysplasia surveillance at time of diagnosis and annually thereafter. Patients with PSC-IBD are at increased risk of synchronous cancer and treatment decisions should take this into account.
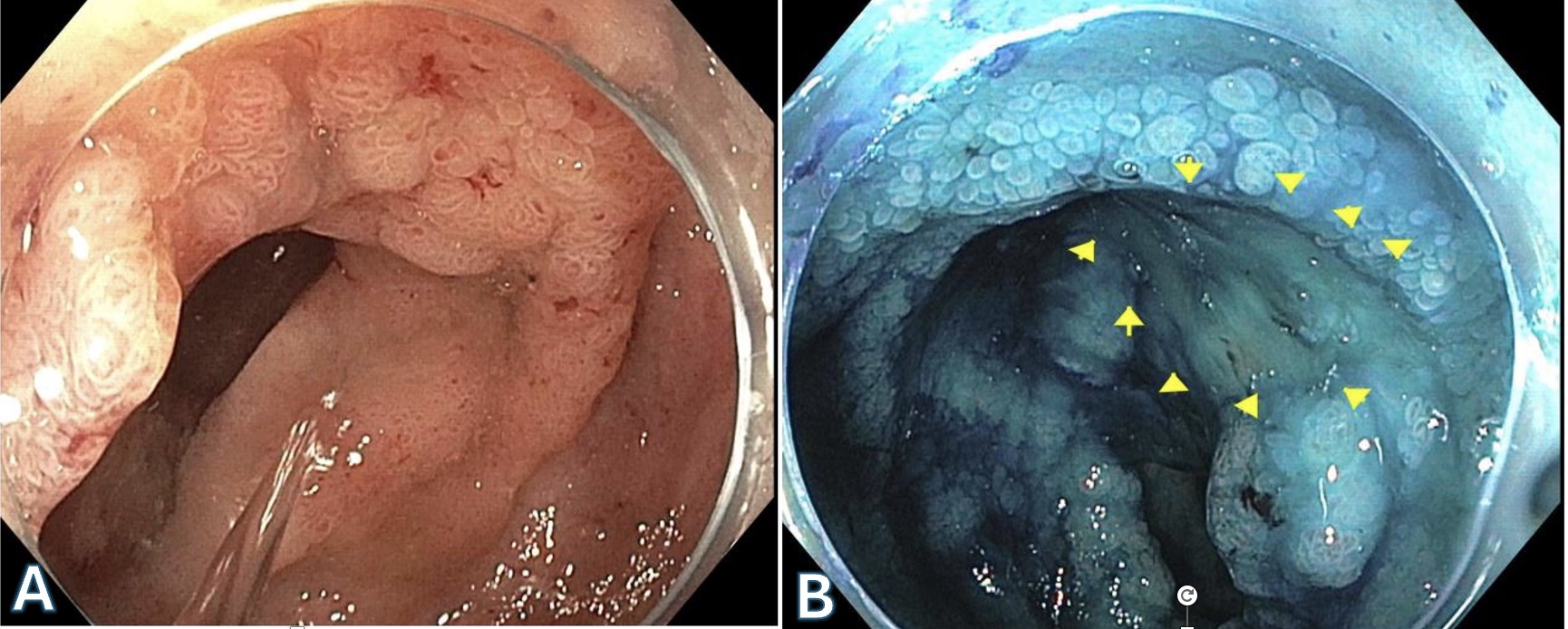
Figure: Figure A. Lesion at the hepatic flexure before chromoendoscopy
Figure B. Lesion at the hepatic flexure after chromoendoscopy showing loss of mucosal surface and an area of central depression
Figure B. Lesion at the hepatic flexure after chromoendoscopy showing loss of mucosal surface and an area of central depression
Disclosures:
Mary Sullivan indicated no relevant financial relationships.
Gianna Stoleru indicated no relevant financial relationships.
Esteban Figueroa: Abbvie – Speakers Bureau.
Mary Sullivan, MD1, Gianna Stoleru, MD2, Esteban Figueroa, MD1. P4430 - Dysplasia Surveillance in PSC-IBD; A Case For Concern, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
