Tuesday Poster Session
Category: IBD
P4438 - A Rare Case of Late Onset IBD Lacking Histologic Evidence of Chronic Inflammation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rebhi Rabah, MD
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Rebhi Rabah, MD1, Kian Bagheri, MD2, Fariha Chowdhury, MD3, Sonny Caceres, MD2, Michael Coles, DO2, Yaniuska Lescaille, MD, MPH2
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3Garnet Health Medical Center, Merrick, NY
Introduction: Both lymphoproliferative disorders (LPDs) and Inflammatory bowel disease (IBD), can present with rectal bleeding that typically involve endoscopic and histologic evidence of inflammatory chronicity. Although B-cell proliferation in IBD is usually associated with inflammation, there were documented cases of LPDs in IBD patients that may present without significant inflammation. A lack of typical features in the pathology can result in misdiagnosis and incorrect treatment plans. We present a case of IBD lacking signs of chronic inflammation in the absence of LPDs.
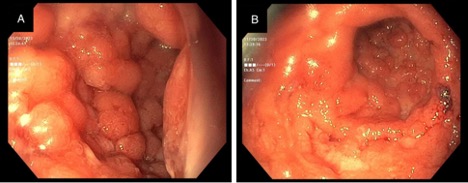
Case Description/Methods: A 61-year-old male with a history of hypertension and diabetes presented with rectal bleeding. Prior to admission, the patient underwent colonoscopy/EGD, which revealed hemorrhoids and severe diffuse inflammation with ulcers in the rectosigmoid colon. Biopsies showed abnormal B cell proliferation with no evidence of chronic inflammation. Serologic workup revealed Strongyloides antibody positivity and he was treated accordingly with Ivermectin. Despite treatment, he had continued hematochezia and associated transfusion-dependent anemia. A repeat flex sigmoidoscopy revealed no therapeutic response to anthelmintic therapy with severe diffuse rectosigmoid inflammation. The biopsy revealed lymphoblastic plasmacytic infiltration but no evidence of chronic inflammation. He was started on IV methylprednisolone, but inflammatory markers continued to increase. A working diagnosis of UC was made, and he was started on Infliximab. Inflammatory markers and symptoms improved. The hospital course was complicated by septic shock secondary to a sacral ulcer, and the patient eventually passed away.
Discussion: Cognizance and timely detection of atypical histological features is imperative as IBD increases worldwide. Delayed detection of IBD is associated with increased rates of abdominal surgeries, worsened prognosis, and increased risk of complications. Here, we saw atypical features of IBD given a rather benign colonic mucosa with ulceration, mild acute inflammation, and lymphoplasmacytic infiltrate. Basal cell plasmacytosis and neutrophils were present, but crypt architecture was normal, which suggests a more acute disease pathology. A smaller subset of patients present without the typical histopathologic evidence of chronicity. However, basal cell plasmacytosis can suggest IBD, especially in the early stages, and one should maintain a high clinical index of suspicion for an IBD diagnosis when these findings are noted.
Disclosures:
Rebhi Rabah, MD1, Kian Bagheri, MD2, Fariha Chowdhury, MD3, Sonny Caceres, MD2, Michael Coles, DO2, Yaniuska Lescaille, MD, MPH2. P4438 - A Rare Case of Late Onset IBD Lacking Histologic Evidence of Chronic Inflammation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3Garnet Health Medical Center, Merrick, NY
Introduction: Both lymphoproliferative disorders (LPDs) and Inflammatory bowel disease (IBD), can present with rectal bleeding that typically involve endoscopic and histologic evidence of inflammatory chronicity. Although B-cell proliferation in IBD is usually associated with inflammation, there were documented cases of LPDs in IBD patients that may present without significant inflammation. A lack of typical features in the pathology can result in misdiagnosis and incorrect treatment plans. We present a case of IBD lacking signs of chronic inflammation in the absence of LPDs.
Case Description/Methods: A 61-year-old male with a history of hypertension and diabetes presented with rectal bleeding. Prior to admission, the patient underwent colonoscopy/EGD, which revealed hemorrhoids and severe diffuse inflammation with ulcers in the rectosigmoid colon. Biopsies showed abnormal B cell proliferation with no evidence of chronic inflammation. Serologic workup revealed Strongyloides antibody positivity and he was treated accordingly with Ivermectin. Despite treatment, he had continued hematochezia and associated transfusion-dependent anemia. A repeat flex sigmoidoscopy revealed no therapeutic response to anthelmintic therapy with severe diffuse rectosigmoid inflammation. The biopsy revealed lymphoblastic plasmacytic infiltration but no evidence of chronic inflammation. He was started on IV methylprednisolone, but inflammatory markers continued to increase. A working diagnosis of UC was made, and he was started on Infliximab. Inflammatory markers and symptoms improved. The hospital course was complicated by septic shock secondary to a sacral ulcer, and the patient eventually passed away.
Discussion: Cognizance and timely detection of atypical histological features is imperative as IBD increases worldwide. Delayed detection of IBD is associated with increased rates of abdominal surgeries, worsened prognosis, and increased risk of complications. Here, we saw atypical features of IBD given a rather benign colonic mucosa with ulceration, mild acute inflammation, and lymphoplasmacytic infiltrate. Basal cell plasmacytosis and neutrophils were present, but crypt architecture was normal, which suggests a more acute disease pathology. A smaller subset of patients present without the typical histopathologic evidence of chronicity. However, basal cell plasmacytosis can suggest IBD, especially in the early stages, and one should maintain a high clinical index of suspicion for an IBD diagnosis when these findings are noted.
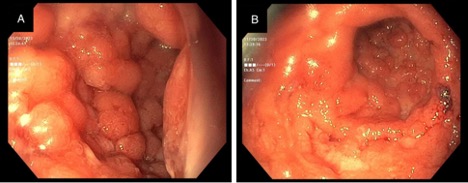
Figure: Figure 1. Flex sigmoidoscopy images revealing diffuse severe inflammation in sigmoid colon (A) and rectum (B).
Disclosures:
Rebhi Rabah indicated no relevant financial relationships.
Kian Bagheri indicated no relevant financial relationships.
Fariha Chowdhury indicated no relevant financial relationships.
Sonny Caceres indicated no relevant financial relationships.
Michael Coles indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Rebhi Rabah, MD1, Kian Bagheri, MD2, Fariha Chowdhury, MD3, Sonny Caceres, MD2, Michael Coles, DO2, Yaniuska Lescaille, MD, MPH2. P4438 - A Rare Case of Late Onset IBD Lacking Histologic Evidence of Chronic Inflammation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
