Tuesday Poster Session
Category: IBD
P4440 - A Case of Strongyloidiasis Masquerading as Ulcerative Colitis Flare
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
Stephanie M. Woo, MD
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Stephanie M. Woo, MD1, Wen Chen, MD2, Debra Benator, MD2, Uni Wong, MD2, Marianna Papademetriou, MD3
1MedStar Georgetown University Hospital, Washington, DC; 2U.S. Department of Veterans Affairs, Washington, DC; 3Washington DC VA Medical Center, Washington, DC
Introduction: Strongyloidiasis is caused by the helminth Strongyloides stercoralis and transmitted by skin contact with contaminated soil. Here we report a case of Strongyloides hyperinfection after treatment for Ulcerative Colitis (UC).
Case Description/Methods: A 59-year-old male veteran with UC, chronic nausea, and restrictive lung disease presented with recurrent diarrhea. The diagnosis of UC was established two years prior with bloody diarrhea, fecal calprotectin (FCP) of 5100mg/g, pancolitis on colonoscopy and chronic active cryptitis on histology. After vedolizumab was initiated, he achieved clinical and endoscopic remission with FCP improved to 200mg/g. He later had recurrence of diarrhea found to be from Shigella and Campylobacter on separate occasions, both treated with resolution of symptoms. Diarrhea recurred again several weeks later. FCP increased to 1180 mg/g and Clostridium Difficile PCR was negative. Sigmoidoscopy showed mild proctitis with chronic active inflammation on histology. Vedolizumab was switched to infliximab. However, his diarrhea worsened along with nausea and vomiting. Stool studies showed Campylobacter was again positive, Shigella was negative, and Clostridium difficile was negative. Restaging sigmoidoscopy showed persistent mild proctitis and upper endoscopy demonstrated duodenitis. Duodenal and rectal biopsies demonstrated Strongyloides larvae in crypts. Strongyloidies antibody later returned positive. Infliximab infusion was held and his symptoms resolved after initiation of ivermectin.
Discussion: Strongyloidiasis can mimic inflammatory bowel disease (IBD). There are reports of patients misdiagnosed with IBD initiated on immunotherapy who develop disseminated strongyloidiasis. Other reports show patients with concomitant IBD and strongyloidiasis who improve with eradication of their infection. Our patient’s initial improvement in symptoms and inflammatory markers with UC treatment leads us to suspect he has underlying UC and later developed strongyloidiasis. Due to multiple opportunistic infections, he was tested for HIV, CVID and HTLV which were both negative. This case is unique since our patient had frequent infections from various pathogens, which obscured his clinical picture, emphasizing the importance of not only bacterial and viral infections but parasitic infections as well, particularly in patients with IBD. Duodenal biopsies are highly sensitive for strongyloides so upper endoscopy should be performed along with antibody if it is on the differential.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Stephanie M. Woo, MD1, Wen Chen, MD2, Debra Benator, MD2, Uni Wong, MD2, Marianna Papademetriou, MD3. P4440 - A Case of Strongyloidiasis Masquerading as Ulcerative Colitis Flare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2U.S. Department of Veterans Affairs, Washington, DC; 3Washington DC VA Medical Center, Washington, DC
Introduction: Strongyloidiasis is caused by the helminth Strongyloides stercoralis and transmitted by skin contact with contaminated soil. Here we report a case of Strongyloides hyperinfection after treatment for Ulcerative Colitis (UC).
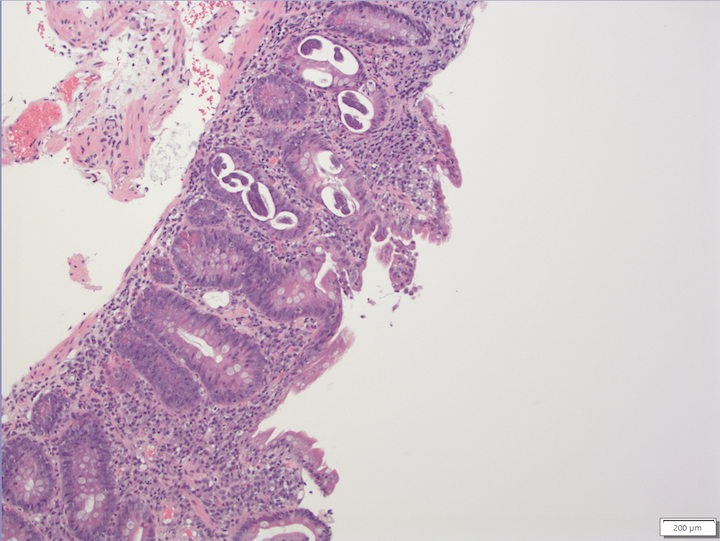
Case Description/Methods: A 59-year-old male veteran with UC, chronic nausea, and restrictive lung disease presented with recurrent diarrhea. The diagnosis of UC was established two years prior with bloody diarrhea, fecal calprotectin (FCP) of 5100mg/g, pancolitis on colonoscopy and chronic active cryptitis on histology. After vedolizumab was initiated, he achieved clinical and endoscopic remission with FCP improved to 200mg/g. He later had recurrence of diarrhea found to be from Shigella and Campylobacter on separate occasions, both treated with resolution of symptoms. Diarrhea recurred again several weeks later. FCP increased to 1180 mg/g and Clostridium Difficile PCR was negative. Sigmoidoscopy showed mild proctitis with chronic active inflammation on histology. Vedolizumab was switched to infliximab. However, his diarrhea worsened along with nausea and vomiting. Stool studies showed Campylobacter was again positive, Shigella was negative, and Clostridium difficile was negative. Restaging sigmoidoscopy showed persistent mild proctitis and upper endoscopy demonstrated duodenitis. Duodenal and rectal biopsies demonstrated Strongyloides larvae in crypts. Strongyloidies antibody later returned positive. Infliximab infusion was held and his symptoms resolved after initiation of ivermectin.
Discussion: Strongyloidiasis can mimic inflammatory bowel disease (IBD). There are reports of patients misdiagnosed with IBD initiated on immunotherapy who develop disseminated strongyloidiasis. Other reports show patients with concomitant IBD and strongyloidiasis who improve with eradication of their infection. Our patient’s initial improvement in symptoms and inflammatory markers with UC treatment leads us to suspect he has underlying UC and later developed strongyloidiasis. Due to multiple opportunistic infections, he was tested for HIV, CVID and HTLV which were both negative. This case is unique since our patient had frequent infections from various pathogens, which obscured his clinical picture, emphasizing the importance of not only bacterial and viral infections but parasitic infections as well, particularly in patients with IBD. Duodenal biopsies are highly sensitive for strongyloides so upper endoscopy should be performed along with antibody if it is on the differential.
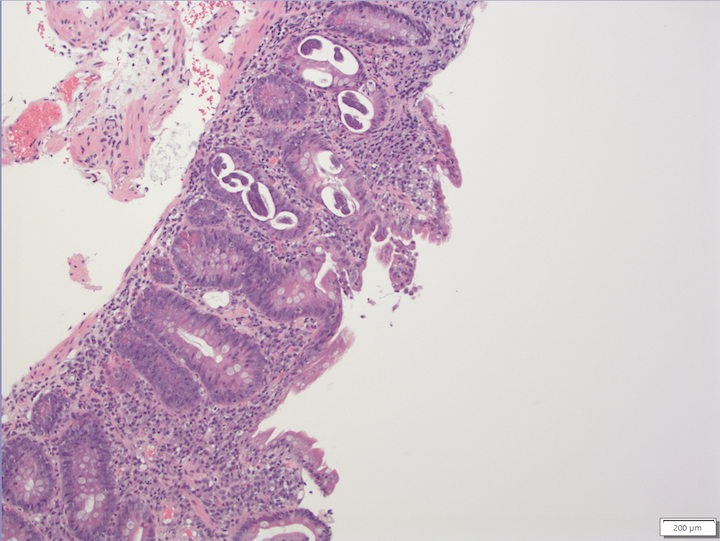
Figure: Strongyloides stercoralis in the duodenum
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Stephanie Woo indicated no relevant financial relationships.
Wen Chen indicated no relevant financial relationships.
Debra Benator indicated no relevant financial relationships.
Uni Wong indicated no relevant financial relationships.
Marianna Papademetriou indicated no relevant financial relationships.
Stephanie M. Woo, MD1, Wen Chen, MD2, Debra Benator, MD2, Uni Wong, MD2, Marianna Papademetriou, MD3. P4440 - A Case of Strongyloidiasis Masquerading as Ulcerative Colitis Flare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
