Tuesday Poster Session
Category: IBD
P4337 - Clinical Outcomes of COVID-19 in Patients With Inflammatory Bowel Disease: Latest Insights From the National Inpatient Sample
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Muhammad Jahanzaib Khan, MD
Mather Hospital, Northwell Health
New York, NY
Presenting Author(s)
Muhammad Jahanzaib Khan, MD1, Mohamad Sharbatji, MD2, Hameed Ullah, MD3, Hasan S. Raza, MD4, Saeed Ali, MD5, Ramona Rajapakse, MD6
1Mather Hospital, Northwell Health, New York, NY; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3Saint Luke's Hospital, St. Louis, MO; 4University of Illinois, Chicago, IL; 5AdventHealth, Orlando, FL; 6Northwell Health, Port Jefferson, NY
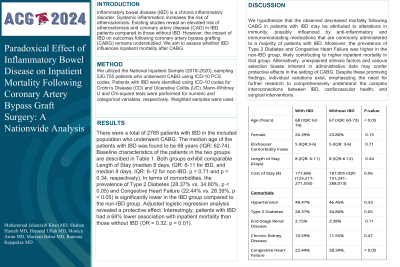
Introduction: Inflammatory bowel disease (IBD) patients are speculated to have increased COVID-19 complications due to immune dysfunction and immunomodulatory therapies, but the impact remains unclear. Existing studies show mixed results on the severity of COVID-19 in IBD patients. This study compares the clinical outcomes of COVID-19 patients with and without IBD using the latest National Inpatient Sample (NIS) data.
Methods: We conducted a retrospective analysis using the NIS database (2020-2021), sampling 2,573,077 patients hospitalized with a principal diagnosis of COVID-19 using ICD-10 codes. Patients with IBD were identified using ICD-10 codes for both Ulcerative Colitis (UC) and Crohn's Disease (CD). Baseline characteristics, including age, gender, Charlson Comorbidity Index (CCI), and race, were analyzed. Key outcomes assessed were all-cause inpatient mortality, resource utilization, development of acute kidney injury (AKI), and the need for ICU admission. Proportions and means were compared using the chi-square test and Student’s t-test, respectively. Univariate analysis was used to generate unadjusted odds ratios (OR), and multivariate linear and logistic regression models were then constructed to calculate adjusted odds ratios (aOR) for continuous and categorical outcomes, respectively.
Results: There were a total of 14,409 (0.56%) patients diagnosed with IBD in the included population. There was a significantly higher proportion of female patients in the IBD group compared to the non-IBD group (53.32% vs. 47.30%, p< 0.01). Baseline characteristics of the patients in the two groups are described in Table 1. Outcomes revealed no significant difference in mortality between IBD (10.82%) and non-IBD (11.27%) patients (aOR 1.05, p=0.44). ICU admission rates were similar (IBD: 10.79%, non-IBD: 10.45%, aOR 1.13, p=0.06). However, AKI was significantly higher in the IBD group (26.14% vs. 24.79%, aOR 1.17, p< 0.01). Mean length of stay (LOS) was marginally longer for IBD patients (7.92 days vs. 7.77 days, coefficient 0.34, p< 0.05).
Discussion: Our study concludes that aside from a higher incidence of AKI, IBD does not significantly worsen clinical outcomes in COVID-19 patients. These results align with previous research, reinforcing the evidence that IBD may not notably increase the risk of adverse outcomes from COVID-19. However, larger, multicenter studies with more comprehensive data are needed to validate our findings and deepen the understanding of IBD's impact on COVID-19 outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Jahanzaib Khan, MD1, Mohamad Sharbatji, MD2, Hameed Ullah, MD3, Hasan S. Raza, MD4, Saeed Ali, MD5, Ramona Rajapakse, MD6. P4337 - Clinical Outcomes of COVID-19 in Patients With Inflammatory Bowel Disease: Latest Insights From the National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mather Hospital, Northwell Health, New York, NY; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3Saint Luke's Hospital, St. Louis, MO; 4University of Illinois, Chicago, IL; 5AdventHealth, Orlando, FL; 6Northwell Health, Port Jefferson, NY
Introduction: Inflammatory bowel disease (IBD) patients are speculated to have increased COVID-19 complications due to immune dysfunction and immunomodulatory therapies, but the impact remains unclear. Existing studies show mixed results on the severity of COVID-19 in IBD patients. This study compares the clinical outcomes of COVID-19 patients with and without IBD using the latest National Inpatient Sample (NIS) data.
Methods: We conducted a retrospective analysis using the NIS database (2020-2021), sampling 2,573,077 patients hospitalized with a principal diagnosis of COVID-19 using ICD-10 codes. Patients with IBD were identified using ICD-10 codes for both Ulcerative Colitis (UC) and Crohn's Disease (CD). Baseline characteristics, including age, gender, Charlson Comorbidity Index (CCI), and race, were analyzed. Key outcomes assessed were all-cause inpatient mortality, resource utilization, development of acute kidney injury (AKI), and the need for ICU admission. Proportions and means were compared using the chi-square test and Student’s t-test, respectively. Univariate analysis was used to generate unadjusted odds ratios (OR), and multivariate linear and logistic regression models were then constructed to calculate adjusted odds ratios (aOR) for continuous and categorical outcomes, respectively.
Results: There were a total of 14,409 (0.56%) patients diagnosed with IBD in the included population. There was a significantly higher proportion of female patients in the IBD group compared to the non-IBD group (53.32% vs. 47.30%, p< 0.01). Baseline characteristics of the patients in the two groups are described in Table 1. Outcomes revealed no significant difference in mortality between IBD (10.82%) and non-IBD (11.27%) patients (aOR 1.05, p=0.44). ICU admission rates were similar (IBD: 10.79%, non-IBD: 10.45%, aOR 1.13, p=0.06). However, AKI was significantly higher in the IBD group (26.14% vs. 24.79%, aOR 1.17, p< 0.01). Mean length of stay (LOS) was marginally longer for IBD patients (7.92 days vs. 7.77 days, coefficient 0.34, p< 0.05).
Discussion: Our study concludes that aside from a higher incidence of AKI, IBD does not significantly worsen clinical outcomes in COVID-19 patients. These results align with previous research, reinforcing the evidence that IBD may not notably increase the risk of adverse outcomes from COVID-19. However, larger, multicenter studies with more comprehensive data are needed to validate our findings and deepen the understanding of IBD's impact on COVID-19 outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Mohamad Sharbatji indicated no relevant financial relationships.
Hameed Ullah indicated no relevant financial relationships.
Hasan Raza indicated no relevant financial relationships.
Saeed Ali indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Muhammad Jahanzaib Khan, MD1, Mohamad Sharbatji, MD2, Hameed Ullah, MD3, Hasan S. Raza, MD4, Saeed Ali, MD5, Ramona Rajapakse, MD6. P4337 - Clinical Outcomes of COVID-19 in Patients With Inflammatory Bowel Disease: Latest Insights From the National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
