Tuesday Poster Session
Category: IBD
P4345 - The Cecal Patch in Ulcerative Proctitis – A Harbinger of Disease Progression or Merely an Incidental Finding?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Laura Sahyoun, MD
New York-Presbyterian Hospital/Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Laura Sahyoun, MD1, Esther Liu, MD2, Robert Battat, MD3, Randy Longman, MD, PhD4, Ellen Scherl, MD1, Dana J. Lukin, MD5
1New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Centre Hospitalier de l'Université de Montréal, Montreal, PQ, Canada; 4Weill Cornell Medicine, New York, NY; 5Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY
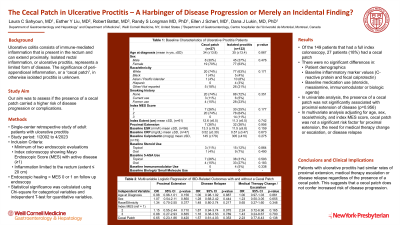
Introduction: Ulcerative colitis classically consists of immune-mediated inflammation that is present in the rectum and can extend proximally in a continuous matter. Isolated rectal inflammation, or ulcerative proctitis, represents a limited form of disease that is not associated with increased risk of dysplasia. Existing literature is sparse and conflicting on the significance of peri-appendiceal inflammation, or a “cecal patch”, in otherwise isolated proctitis. Our aim was to assess if the presence of a cecal patch carried a higher risk of disease progression or complications.
Methods: This is a single-center retrospective study of adult patients with ulcerative proctitis treated from 1/2002 to 4/2023. Patients were included in the study if they had a minimum of two endoscopic evaluations, with index colonoscopy showing Mayo Endoscopic Score (MES) with active disease (≥1) that was limited to the rectum (extent ≤ 20 cm). Endoscopic healing was defined as MES 0 or 1 on follow up endoscopy. Statistical significance was calculated using Chi-square for categorical variables and independent T-test for quantitative variables.
Results: Of the 200 patients with isolated proctitis, 25 had a cecal patch present at index colonoscopy. Between those with a cecal patch and those without, there were no significant differences in patient demographics, baseline inflammatory marker values (C-reactive protein and fecal calprotectin), or baseline medication use (steroids, mesalamine, immunomodulator or biologic agents). In univariate analysis, the presence of a cecal patch was not significantly associated with proximal extension of disease (p=0.699). In multivariate analysis adjusting for age, sex, race/ethnicity, and index MES score, cecal patch was not a significant risk factor for proximal extension, the need for medical therapy change or escalation, or disease relapse (Table 1).
Discussion: Patients with ulcerative proctitis had similar rates of proximal extension, medical therapy escalation or disease relapse regardless of the presence of a cecal patch. This suggests that a cecal patch does not confer increased risk of disease progression.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Laura Sahyoun, MD1, Esther Liu, MD2, Robert Battat, MD3, Randy Longman, MD, PhD4, Ellen Scherl, MD1, Dana J. Lukin, MD5. P4345 - The Cecal Patch in Ulcerative Proctitis – A Harbinger of Disease Progression or Merely an Incidental Finding?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Centre Hospitalier de l'Université de Montréal, Montreal, PQ, Canada; 4Weill Cornell Medicine, New York, NY; 5Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY
Introduction: Ulcerative colitis classically consists of immune-mediated inflammation that is present in the rectum and can extend proximally in a continuous matter. Isolated rectal inflammation, or ulcerative proctitis, represents a limited form of disease that is not associated with increased risk of dysplasia. Existing literature is sparse and conflicting on the significance of peri-appendiceal inflammation, or a “cecal patch”, in otherwise isolated proctitis. Our aim was to assess if the presence of a cecal patch carried a higher risk of disease progression or complications.
Methods: This is a single-center retrospective study of adult patients with ulcerative proctitis treated from 1/2002 to 4/2023. Patients were included in the study if they had a minimum of two endoscopic evaluations, with index colonoscopy showing Mayo Endoscopic Score (MES) with active disease (≥1) that was limited to the rectum (extent ≤ 20 cm). Endoscopic healing was defined as MES 0 or 1 on follow up endoscopy. Statistical significance was calculated using Chi-square for categorical variables and independent T-test for quantitative variables.
Results: Of the 200 patients with isolated proctitis, 25 had a cecal patch present at index colonoscopy. Between those with a cecal patch and those without, there were no significant differences in patient demographics, baseline inflammatory marker values (C-reactive protein and fecal calprotectin), or baseline medication use (steroids, mesalamine, immunomodulator or biologic agents). In univariate analysis, the presence of a cecal patch was not significantly associated with proximal extension of disease (p=0.699). In multivariate analysis adjusting for age, sex, race/ethnicity, and index MES score, cecal patch was not a significant risk factor for proximal extension, the need for medical therapy change or escalation, or disease relapse (Table 1).
Discussion: Patients with ulcerative proctitis had similar rates of proximal extension, medical therapy escalation or disease relapse regardless of the presence of a cecal patch. This suggests that a cecal patch does not confer increased risk of disease progression.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Laura Sahyoun indicated no relevant financial relationships.
Esther Liu indicated no relevant financial relationships.
Robert Battat: Abbvie – Advisory Committee/Board Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Consultant, Speakers Bureau. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Prometheus Laboratories – Advisory Committee/Board Member, Consultant, Speakers Bureau. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Randy Longman: Bristol Myers Squibb – Consultant. Pfizer – Consultant.
Ellen Scherl: Abbvie – Consultant, Speakers Bureau. BMS – Consultant, Speakers Bureau. Johnson and Johnson – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Dana J. Lukin: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. AltruBio – Consultant. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Janssen – Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Consultant. Palatin Technologies – Consultant. Pfizer – Consultant. Prometheus Laboratories – Consultant. PSI – Consultant. Takeda – Consultant, Grant/Research Support.
Laura Sahyoun, MD1, Esther Liu, MD2, Robert Battat, MD3, Randy Longman, MD, PhD4, Ellen Scherl, MD1, Dana J. Lukin, MD5. P4345 - The Cecal Patch in Ulcerative Proctitis – A Harbinger of Disease Progression or Merely an Incidental Finding?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
