Tuesday Poster Session
Category: IBD
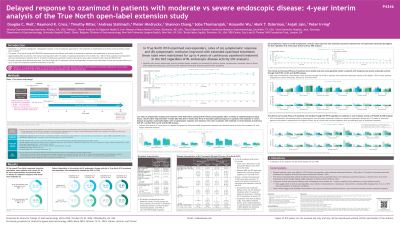
P4346 - Delayed Response to Ozanimod in Patients with Moderate vs Severe Endoscopic Disease: 4-Year Interim Analysis of the True North Open-Label Extension Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Douglas Wolf, MD, FACG
Center for Crohn’s Disease & Ulcerative Colitis, Atlanta Gastroenterology Associates
Atlanta, GA
Presenting Author(s)
Douglas C. Wolf, MD, FACG1, Raymond K. Cross, MD, MS, FACG2, Timothy E. Ritter, MD3, Andreas Stallmach, MD4, Pieter Hindryckx, MD, PhD5, Shannon Chang, MD6, Soba Tharmarajah, PharmD7, Hsiuanlin Wu, MS7, Mark T. Osterman, MD7, Anjali Jain, PhD7, Peter M.. Irving, MA, MD8
1Center for Crohn’s Disease & Ulcerative Colitis, Atlanta Gastroenterology Associates, Atlanta, GA; 2Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD; 3GI Alliance, Southlake, TX; 4Jena University Hospital, Jena, Hamburg, Germany; 5University Hospital Ghent, Ghent, Limburg, Belgium; 6New York University Langone Health, New York, NY; 7Bristol Myers Squibb, Princeton, NJ; 8Guy’s and St. Thomas’ NHS Foundation Trust, London, England, United Kingdom
Introduction: Ozanimod (OZA) is approved for the treatment (tx) of moderately to severely active ulcerative colitis (UC). About 30% of patients (pts) were clinical nonresponders (NRs) after 10 wk of OZA tx in the phase 3 True North (TN) study (NCT02435992), but ~50% of these pts achieved symptomatic response after 5–10 wk of additional OZA tx during the open-label extension (OLE) study (NCT02531126).
Methods: This analysis evaluated the impact of TN baseline (BL) endoscopic disease activity on the durability of OZA response in Week (W) 10 OZA clinical NRs after extended induction during the OLE up to 4 years (OLE W190). Pts were categorized by BL Mayo endoscopy subscore (MES) as moderate (MOD; MES=2) or severe (SEV; MES=3). Efficacy was assessed through OLE W190 using observed case (OC) and nonresponder imputation (NRI) analyses.
Results: Of the 226 W10 OZA clinical NRs who entered the OLE, 67 had MOD and 159 had SEV endoscopic disease at BL. Pt characteristics were generally similar between groups, but more pts with SEV vs MOD endoscopic activity had prior immunomodulator (52.8% vs 34.3%), anti–tumor necrosis factor (TNF; 45.9% vs 25.4%), or non–anti-TNF biologic (36.5% vs 19.4%) exposure. Some symptomatic response was observed in OZA W10 clinical NRs from BL to W10/OLE entry, which was greater in pts with MOD disease and further improved with extended OZA exposure by OLE W5; similar patterns were observed with symptomatic remission but overall rates were lower (Figure). Symptomatic response and remission rates after OLE W5 were generally similar in MOD and SEV endoscopic activity groups, and rates were maintained throughout the OLE. Likewise, clinical and mucosal efficacy were durable and rates were generally similar between subgroups through OLE W190 (Table). Notably, higher endoscopic improvement rates were achieved through OLE W190 in pts with BL MOD endoscopic activity despite ~50% of these pts progressing to SEV by TN W10. Similar data trends were observed in the NRI analysis.
Discussion: Delayed response to OZA was observed in pts who did not achieve clinical response after 10 wk of OZA therapy, regardless of BL endoscopic activity. W10 NRs with MOD endoscopic activity responded faster with additional OZA exposure, whereas those with SEV endoscopic activity needed longer exposure to OZA to achieve similar efficacy rates that were durable with continuous OZA exposure. These results suggest that some pts may require a longer induction on OZA but ultimately maintain durable OZA response.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Douglas C. Wolf, MD, FACG1, Raymond K. Cross, MD, MS, FACG2, Timothy E. Ritter, MD3, Andreas Stallmach, MD4, Pieter Hindryckx, MD, PhD5, Shannon Chang, MD6, Soba Tharmarajah, PharmD7, Hsiuanlin Wu, MS7, Mark T. Osterman, MD7, Anjali Jain, PhD7, Peter M.. Irving, MA, MD8. P4346 - Delayed Response to Ozanimod in Patients with Moderate vs Severe Endoscopic Disease: 4-Year Interim Analysis of the True North Open-Label Extension Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Center for Crohn’s Disease & Ulcerative Colitis, Atlanta Gastroenterology Associates, Atlanta, GA; 2Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD; 3GI Alliance, Southlake, TX; 4Jena University Hospital, Jena, Hamburg, Germany; 5University Hospital Ghent, Ghent, Limburg, Belgium; 6New York University Langone Health, New York, NY; 7Bristol Myers Squibb, Princeton, NJ; 8Guy’s and St. Thomas’ NHS Foundation Trust, London, England, United Kingdom
Introduction: Ozanimod (OZA) is approved for the treatment (tx) of moderately to severely active ulcerative colitis (UC). About 30% of patients (pts) were clinical nonresponders (NRs) after 10 wk of OZA tx in the phase 3 True North (TN) study (NCT02435992), but ~50% of these pts achieved symptomatic response after 5–10 wk of additional OZA tx during the open-label extension (OLE) study (NCT02531126).
Methods: This analysis evaluated the impact of TN baseline (BL) endoscopic disease activity on the durability of OZA response in Week (W) 10 OZA clinical NRs after extended induction during the OLE up to 4 years (OLE W190). Pts were categorized by BL Mayo endoscopy subscore (MES) as moderate (MOD; MES=2) or severe (SEV; MES=3). Efficacy was assessed through OLE W190 using observed case (OC) and nonresponder imputation (NRI) analyses.
Results: Of the 226 W10 OZA clinical NRs who entered the OLE, 67 had MOD and 159 had SEV endoscopic disease at BL. Pt characteristics were generally similar between groups, but more pts with SEV vs MOD endoscopic activity had prior immunomodulator (52.8% vs 34.3%), anti–tumor necrosis factor (TNF; 45.9% vs 25.4%), or non–anti-TNF biologic (36.5% vs 19.4%) exposure. Some symptomatic response was observed in OZA W10 clinical NRs from BL to W10/OLE entry, which was greater in pts with MOD disease and further improved with extended OZA exposure by OLE W5; similar patterns were observed with symptomatic remission but overall rates were lower (Figure). Symptomatic response and remission rates after OLE W5 were generally similar in MOD and SEV endoscopic activity groups, and rates were maintained throughout the OLE. Likewise, clinical and mucosal efficacy were durable and rates were generally similar between subgroups through OLE W190 (Table). Notably, higher endoscopic improvement rates were achieved through OLE W190 in pts with BL MOD endoscopic activity despite ~50% of these pts progressing to SEV by TN W10. Similar data trends were observed in the NRI analysis.
Discussion: Delayed response to OZA was observed in pts who did not achieve clinical response after 10 wk of OZA therapy, regardless of BL endoscopic activity. W10 NRs with MOD endoscopic activity responded faster with additional OZA exposure, whereas those with SEV endoscopic activity needed longer exposure to OZA to achieve similar efficacy rates that were durable with continuous OZA exposure. These results suggest that some pts may require a longer induction on OZA but ultimately maintain durable OZA response.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Douglas C. Wolf: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Amgen – Grant/Research Support. Arena/Pfizer – Consultant, Grant/Research Support. Celgene/Bristol Myers Squibb – Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly – Consultant. Genentech – Grant/Research Support. Janssen – Consultant, Grant/Research Support, Speakers Bureau. Takeda – Consultant, Speakers Bureau.
Raymond Cross: AbbVie – Consultant. Adiso – Consultant. Bristol Myers Squibb – Consultant. CorEvitas Registry – Scientific co-director. Fresenius Kabi – Consultant. Fzata – Consultant. IBD Education Group – Executive committee member. Janssen – Consultant, Grant/Research Support. Magellan Health – Consultant. Option Care Health – Consultant. Pfizer – Consultant. Pharmacosmos – Consultant. Samsung Bioepis – Consultant. Sandoz – Consultant. Sebela – Consultant. Takeda – Consultant.
Timothy Ritter: AbbVie – Advisory Committee/Board Member, Speakers Bureau. Ardelyx – Advisory Committee/Board Member. Arena Pharmaceuticals – Advisory Committee/Board Member. Boehringer Ingelheim – Advisory Committee/Board Member. Bristol Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Celgene – Advisory Committee/Board Member. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Ferring – Advisory Committee/Board Member. Ferring/Rebiotix – has served on a Data Adjudication Committee. Genentech (Roche) – Advisory Committee/Board Member. Intercept – Advisory Committee/Board Member. Iterative Scopes – Advisory Committee/Board Member, holds shares in Iterative Scopes. Janssen – Advisory Committee/Board Member, Speakers Bureau. Nestlé/Seres – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Speakers Bureau. Prometheus – Advisory Committee/Board Member. Sanofi – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Andreas Stallmach indicated no relevant financial relationships.
Pieter Hindryckx: Boston Scientific – Consultant, Speakers Bureau. FujiFilm – Consultant, Speakers Bureau. MedWork – Consultant, Speakers Bureau. Viatris – Consultant, Speakers Bureau.
Shannon Chang: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant.
Soba Tharmarajah: Bristol Myers Squibb – Employee.
Hsiuanlin Wu: Bristol Myers Squibb – Employee.
Mark T. Osterman: Bristol Myers Squibb – Employee.
Anjali Jain: Bristol Myers Squibb – Employee.
Peter Irving: AbbVie – Advisory Committee/Board Member, Speakers Bureau. Arena – Advisory Committee/Board Member. Boehringer Ingelheim – Advisory Committee/Board Member. Bristol Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Celgene – Advisory Committee/Board Member, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Dr. Falk Pharma – Speakers Bureau. Eli Lilly – Advisory Committee/Board Member. Ferring – Speakers Bureau. Galapagos – Speakers Bureau. Genentech – Advisory Committee/Board Member. Gilead – Advisory Committee/Board Member, Speakers Bureau. Hospira – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Speakers Bureau. MSD – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Pharmacosmos – Advisory Committee/Board Member. Prometheus Biosciences – Advisory Committee/Board Member. Roche – Advisory Committee/Board Member. Samsung Bioepis – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member, Speakers Bureau. Sapphire Medical – Speakers Bureau. Shire – Speakers Bureau. Takeda – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Tillotts – Speakers Bureau. TopiVert – Advisory Committee/Board Member. VH2 – Advisory Committee/Board Member. Vifor – Advisory Committee/Board Member. Warner Chilcott – Advisory Committee/Board Member, Speakers Bureau.
Douglas C. Wolf, MD, FACG1, Raymond K. Cross, MD, MS, FACG2, Timothy E. Ritter, MD3, Andreas Stallmach, MD4, Pieter Hindryckx, MD, PhD5, Shannon Chang, MD6, Soba Tharmarajah, PharmD7, Hsiuanlin Wu, MS7, Mark T. Osterman, MD7, Anjali Jain, PhD7, Peter M.. Irving, MA, MD8. P4346 - Delayed Response to Ozanimod in Patients with Moderate vs Severe Endoscopic Disease: 4-Year Interim Analysis of the True North Open-Label Extension Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
