Tuesday Poster Session
Category: GI Bleeding
P4256 - Duodenal Varices
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Suhail Sidhu, MD
CHI Health Creighton University Medical Center
Anaheim, CA
Presenting Author(s)
Suhail Sidhu, MD1, Kavitha Vijayasekar, MD2, Syed Mohsin Saghir, MD2, Mohammed Qasswal, MD2, Ahmad Al-Chalabi, MBChB3
1CHI Health Creighton University Medical Center, Fremont, CA; 2CHI Health Creighton University Medical Center, Omaha, NE; 3CHI Health Creighton University Medical Center, Omaha, CA
Introduction: Literature is scarce on the management of ectopic varices. Prior case reports have demonstrated utilizing clips, coils, glue, and TIPS.
Case Description/Methods: A 70-year-old man with a past medical history of hypertension, emphysema, CHF, CKD, T2DM, AFIB on Eliquis presented to the ED for three days of hematochezia and hematemesis. He endorsed dizziness, shortness of breath, and NSAIDs use biweekly. He denied tobacco or ETOH use. Two months ago, the patient underwent EGD, colonoscopy, and capsule endoscopy for evaluation for melena, which were all inconclusive. Physical exam showed conjunctival pallor, dry mucosal membranes, and a capillary refill of >3s.. Initial labs showed hemoglobin of 5.7, creatinine of 1.99, potassium of 6.9, lactate of 14.5, and WBC of 17.4. CTA revealed no active GI bleeding. There was evidence of moderate-sized varices involving the distal duodenum without obvious extravasation, cirrhosis, possible left portal vein thrombosis, and chronic SMV thrombosis with collaterals.
Patient was found to be hypotensive on admission, admitted to the ICU for vasopressor support, and started on prophylactic antibiotics, octreotide, and PPI IV BID. He underwent an emergent upper endoscopy, which revealed a spurting bleed in the D2/D3 area of the duodenum. Three hemostatic clips were placed, which stopped the bleeding. No esophageal or gastric varices were visualized. Hematin was appreciated in the stomach. The patient was kept on octreotide and antibiotics, was extubated without further bleeding, and discharged with a hemoglobin of 8.4. Five days after discharge, the patient presented to the ED with hematochezia and shortness of breath with a hemoglobin of 6.3. A repeat upper endoscopy revealed active bleeding from the same duodenal varix with only one clip present. Two new hemostatic clips were placed along with a sclerosing agent with hemostasis. Due to concern for ongoing bleeding, EUS-guided glue and coiling was performed, after which flow was absent in the duodenal varices on the Doppler exam. The patient was discharged home with a hemoglobin of 10. Several months later the patient was found to have bilateral pulmonary emboli requiring tPA. He suffered a cardiopulmonary arrest, ultimately leading to his demise.
Discussion: Our patient had several interventions and tolerated them well. This case report demonstrates that ectopic varices can be successfully managed via endoscopic interventions. Further studies are necessary to evaluate the most effective approach.
Disclosures:
Suhail Sidhu, MD1, Kavitha Vijayasekar, MD2, Syed Mohsin Saghir, MD2, Mohammed Qasswal, MD2, Ahmad Al-Chalabi, MBChB3. P4256 - Duodenal Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Fremont, CA; 2CHI Health Creighton University Medical Center, Omaha, NE; 3CHI Health Creighton University Medical Center, Omaha, CA
Introduction: Literature is scarce on the management of ectopic varices. Prior case reports have demonstrated utilizing clips, coils, glue, and TIPS.
Case Description/Methods: A 70-year-old man with a past medical history of hypertension, emphysema, CHF, CKD, T2DM, AFIB on Eliquis presented to the ED for three days of hematochezia and hematemesis. He endorsed dizziness, shortness of breath, and NSAIDs use biweekly. He denied tobacco or ETOH use. Two months ago, the patient underwent EGD, colonoscopy, and capsule endoscopy for evaluation for melena, which were all inconclusive. Physical exam showed conjunctival pallor, dry mucosal membranes, and a capillary refill of >3s.. Initial labs showed hemoglobin of 5.7, creatinine of 1.99, potassium of 6.9, lactate of 14.5, and WBC of 17.4. CTA revealed no active GI bleeding. There was evidence of moderate-sized varices involving the distal duodenum without obvious extravasation, cirrhosis, possible left portal vein thrombosis, and chronic SMV thrombosis with collaterals.
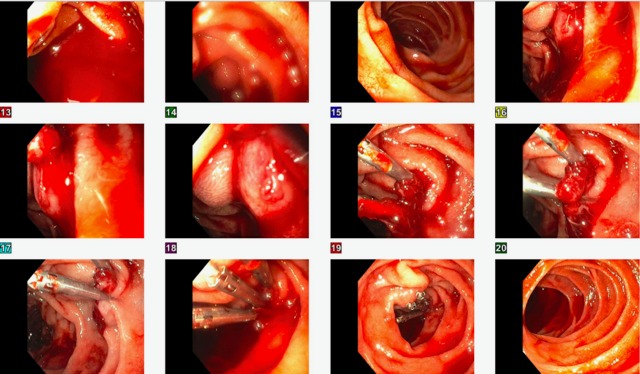
Patient was found to be hypotensive on admission, admitted to the ICU for vasopressor support, and started on prophylactic antibiotics, octreotide, and PPI IV BID. He underwent an emergent upper endoscopy, which revealed a spurting bleed in the D2/D3 area of the duodenum. Three hemostatic clips were placed, which stopped the bleeding. No esophageal or gastric varices were visualized. Hematin was appreciated in the stomach. The patient was kept on octreotide and antibiotics, was extubated without further bleeding, and discharged with a hemoglobin of 8.4. Five days after discharge, the patient presented to the ED with hematochezia and shortness of breath with a hemoglobin of 6.3. A repeat upper endoscopy revealed active bleeding from the same duodenal varix with only one clip present. Two new hemostatic clips were placed along with a sclerosing agent with hemostasis. Due to concern for ongoing bleeding, EUS-guided glue and coiling was performed, after which flow was absent in the duodenal varices on the Doppler exam. The patient was discharged home with a hemoglobin of 10. Several months later the patient was found to have bilateral pulmonary emboli requiring tPA. He suffered a cardiopulmonary arrest, ultimately leading to his demise.
Discussion: Our patient had several interventions and tolerated them well. This case report demonstrates that ectopic varices can be successfully managed via endoscopic interventions. Further studies are necessary to evaluate the most effective approach.
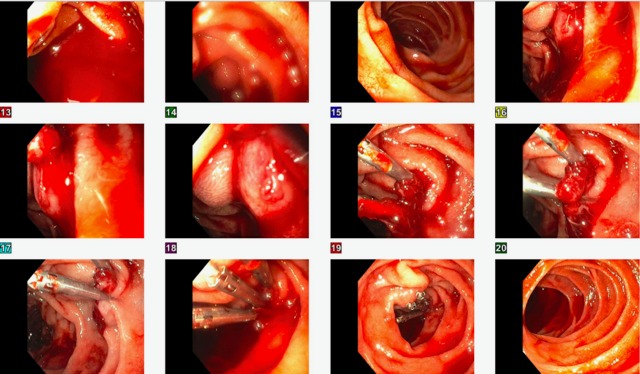
Figure: Index Endoscopy
Disclosures:
Suhail Sidhu indicated no relevant financial relationships.
Kavitha Vijayasekar indicated no relevant financial relationships.
Syed Mohsin Saghir indicated no relevant financial relationships.
Mohammed Qasswal indicated no relevant financial relationships.
Ahmad Al-Chalabi indicated no relevant financial relationships.
Suhail Sidhu, MD1, Kavitha Vijayasekar, MD2, Syed Mohsin Saghir, MD2, Mohammed Qasswal, MD2, Ahmad Al-Chalabi, MBChB3. P4256 - Duodenal Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
