Monday Poster Session
Category: Interventional Endoscopy
P2777 - Endoscopic Ultrasonography-Guided Gastroenterostomy vs Enteral Stenting for Gastric Outlet Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Sahib Singh, MD
Sinai Hospital
Baltimore, MD
Presenting Author(s)
Sahib Singh, MD1, Babu Mohan, MD2, Yash R. Shah, MD3, Vishnu Charan Suresh Kumar, MD4, Ganesh Aswath, MD4, Rakesh Vinayek, MD1, Sudhir Dutta, MD1, Dushyant S. Dahiya, MD5, Sumant Inamdar, MD6, Douglas Adler, MD7, Hassam Ali, MD8, Neil R Sharma, MD, FACG9
1Sinai Hospital, Baltimore, MD; 2Orlando Gastroenterology PA, Orlando, FL; 3Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 4SUNY Upstate Medical University, Syracuse, NY; 5The University of Kansas School of Medicine, Kansas City, KS; 6University of Arkansas for Medical Sciences, Little Rock, AR; 7Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO; 8ECU Health Medical Center, Greenville, NC; 9IOSE. Peak Gastroenterology & Gastrocare Partners., Colorado Springs, CO
Introduction: In patients with gastric outlet obstruction (GOO), clinical studies comparing endoscopic ultrasonography-guided gastroenterostomy (EUS-GE) to enteral stenting (ES) have shown variable results. We conducted a meta-analysis to reconcile the data.
Methods: Online databases were searched for studies evaluating EUS-GE vs ES in patients with GOO. The endpoints of interest were technical success, clinical success, procedure time (minutes), hospital stay (days), need for reintervention, adverse events (AEs) and mortality. Odds ratio (OR) and standardized mean difference (SMD), along with 95% confidence interval (CI) were estimated by performing random effect meta-analysis.
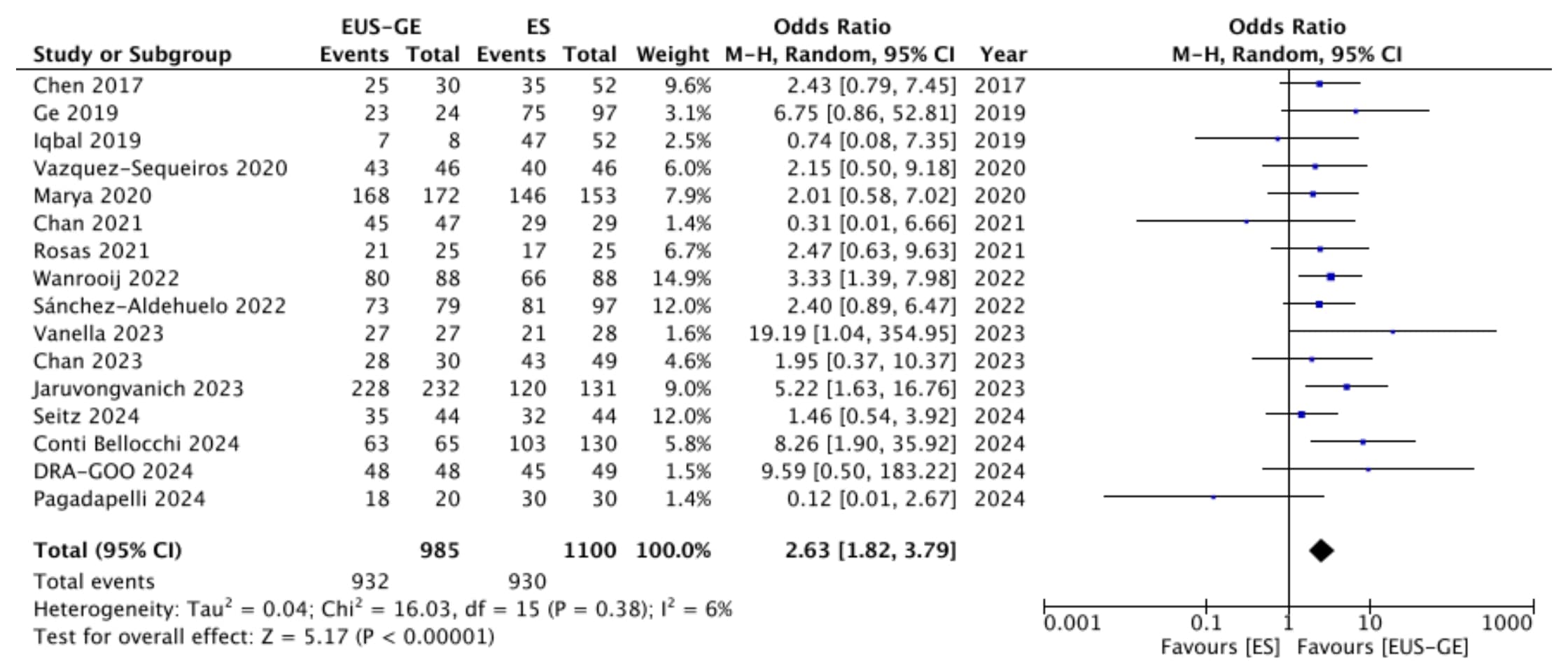
Results: Seventeen studies (1 randomized trial and 16 observational) with a total of 2105 patients (EUS-GE n=1004, ES n=1101) were included in the final analysis. The mean age of the patients was 67 years and 55% were men. EUS-GE had a lower rate of technical success as compared with ES (OR 0.53, 95% CI 0.30 to 0.92, p = 0.02), however clinical success was higher in the EUS-GE group (OR 2.63, 95% CI 1.82 to 3.79, p < 0.00001) (Figure 1). Although procedure time was longer with EUS-GE (SMD 1.45, 95% CI 0.29 to 2.62, p = 0.01), it led to significant reduction in hospital stay (SMD -0.63, 95% CI -1.15 to -0.11, p = 0.02). EUS-GE was associated with decreased reintervention rate (OR 0.13, 95% CI 0.08 to 0.20, p < 0.00001), total AEs (OR 0.51, 95% CI 0.30 to 0.84, p = 0.009) and stent obstruction (OR 0.08, 95% CI 0.02 to 0.36, p = 0.0008). The two groups were comparable in terms of obstructive jaundice/biliary obstruction (OR 0.87, 95% CI 0.21 to 3.55, p = 0.84), cholangitis (OR 0.74, 95% CI 0.28 to 1.99, p = 0.55), pneumonia (OR 0.42, 95% CI 0.11 to 1.59, p = 0.20) and mortality (OR 0.71, 95% CI 0.27 to 1.84, p = 0.48).
Discussion: EUS-GE may be a better therapeutic modality in patients with GOO as compared with ES, due to the higher rate of clinical success, combined with lower reintervention rate and AEs.
Disclosures:
Sahib Singh, MD1, Babu Mohan, MD2, Yash R. Shah, MD3, Vishnu Charan Suresh Kumar, MD4, Ganesh Aswath, MD4, Rakesh Vinayek, MD1, Sudhir Dutta, MD1, Dushyant S. Dahiya, MD5, Sumant Inamdar, MD6, Douglas Adler, MD7, Hassam Ali, MD8, Neil R Sharma, MD, FACG9. P2777 - Endoscopic Ultrasonography-Guided Gastroenterostomy vs Enteral Stenting for Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sinai Hospital, Baltimore, MD; 2Orlando Gastroenterology PA, Orlando, FL; 3Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 4SUNY Upstate Medical University, Syracuse, NY; 5The University of Kansas School of Medicine, Kansas City, KS; 6University of Arkansas for Medical Sciences, Little Rock, AR; 7Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO; 8ECU Health Medical Center, Greenville, NC; 9IOSE. Peak Gastroenterology & Gastrocare Partners., Colorado Springs, CO
Introduction: In patients with gastric outlet obstruction (GOO), clinical studies comparing endoscopic ultrasonography-guided gastroenterostomy (EUS-GE) to enteral stenting (ES) have shown variable results. We conducted a meta-analysis to reconcile the data.
Methods: Online databases were searched for studies evaluating EUS-GE vs ES in patients with GOO. The endpoints of interest were technical success, clinical success, procedure time (minutes), hospital stay (days), need for reintervention, adverse events (AEs) and mortality. Odds ratio (OR) and standardized mean difference (SMD), along with 95% confidence interval (CI) were estimated by performing random effect meta-analysis.
Results: Seventeen studies (1 randomized trial and 16 observational) with a total of 2105 patients (EUS-GE n=1004, ES n=1101) were included in the final analysis. The mean age of the patients was 67 years and 55% were men. EUS-GE had a lower rate of technical success as compared with ES (OR 0.53, 95% CI 0.30 to 0.92, p = 0.02), however clinical success was higher in the EUS-GE group (OR 2.63, 95% CI 1.82 to 3.79, p < 0.00001) (Figure 1). Although procedure time was longer with EUS-GE (SMD 1.45, 95% CI 0.29 to 2.62, p = 0.01), it led to significant reduction in hospital stay (SMD -0.63, 95% CI -1.15 to -0.11, p = 0.02). EUS-GE was associated with decreased reintervention rate (OR 0.13, 95% CI 0.08 to 0.20, p < 0.00001), total AEs (OR 0.51, 95% CI 0.30 to 0.84, p = 0.009) and stent obstruction (OR 0.08, 95% CI 0.02 to 0.36, p = 0.0008). The two groups were comparable in terms of obstructive jaundice/biliary obstruction (OR 0.87, 95% CI 0.21 to 3.55, p = 0.84), cholangitis (OR 0.74, 95% CI 0.28 to 1.99, p = 0.55), pneumonia (OR 0.42, 95% CI 0.11 to 1.59, p = 0.20) and mortality (OR 0.71, 95% CI 0.27 to 1.84, p = 0.48).
Discussion: EUS-GE may be a better therapeutic modality in patients with GOO as compared with ES, due to the higher rate of clinical success, combined with lower reintervention rate and AEs.
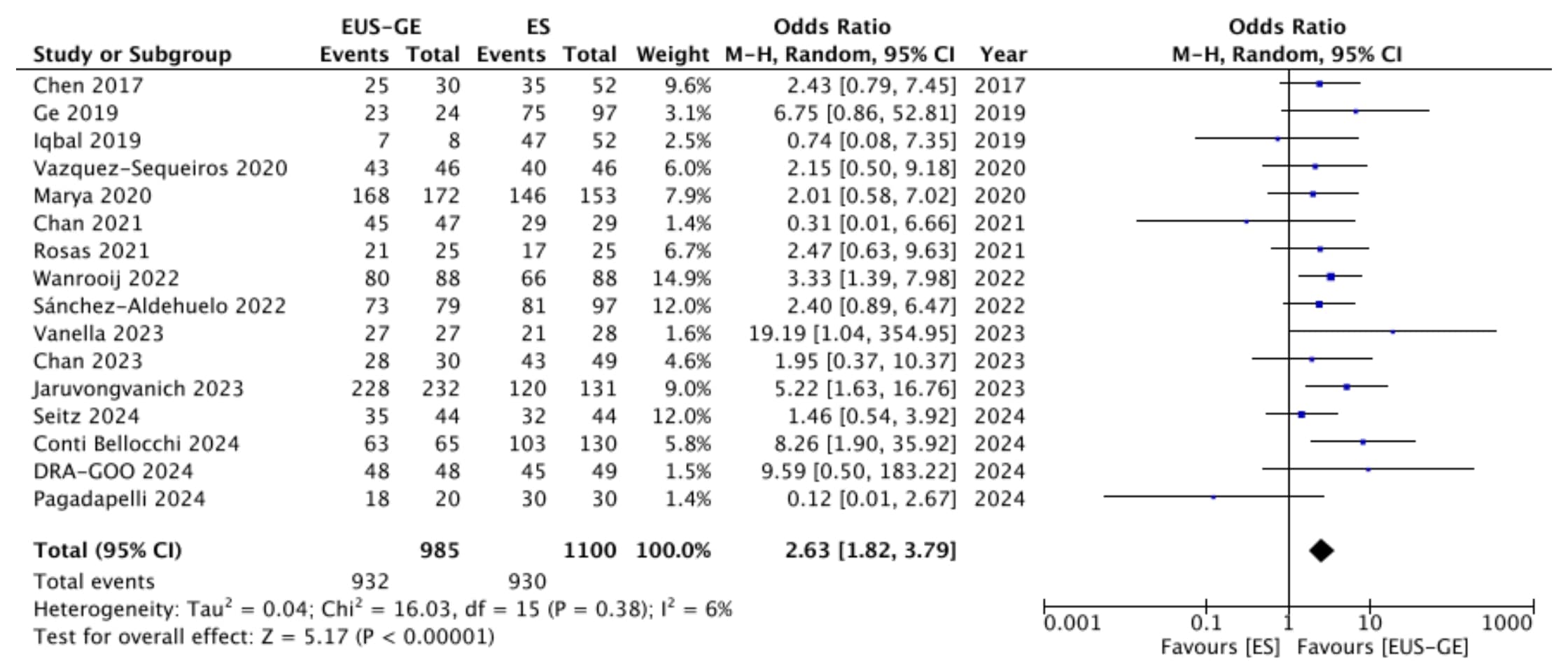
Figure: Clinical success
Disclosures:
Sahib Singh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Vishnu Charan Suresh Kumar indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Rakesh Vinayek indicated no relevant financial relationships.
Sudhir Dutta indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Sumant Inamdar indicated no relevant financial relationships.
Douglas Adler: Boston Scientific and Micro Tech. – Consultant.
Hassam Ali indicated no relevant financial relationships.
Neil R Sharma: Boston Scientific – Consultant. Medtronic – Consultant. Olympus – Consultant. Steris – Consultant.
Sahib Singh, MD1, Babu Mohan, MD2, Yash R. Shah, MD3, Vishnu Charan Suresh Kumar, MD4, Ganesh Aswath, MD4, Rakesh Vinayek, MD1, Sudhir Dutta, MD1, Dushyant S. Dahiya, MD5, Sumant Inamdar, MD6, Douglas Adler, MD7, Hassam Ali, MD8, Neil R Sharma, MD, FACG9. P2777 - Endoscopic Ultrasonography-Guided Gastroenterostomy vs Enteral Stenting for Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
