Monday Poster Session
Category: Interventional Endoscopy
P2783 - Comparative Effectiveness and Safety of Endoscopic Ultrasound-Guided Therapy versus Direct Endoscopic Glue Injection Therapy for Gastric Varices: A Systematic Review and Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Azizullah Beran, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Azizullah Beran, MD1, Mouhand F.H. Mohamed, MD, MSc2, Hazem Abosheaishaa, MD3, Hala Fatima, MD4, Mark A. Gromski, MD1, Mohammad Al-Haddad, MD, FACG1, John M. DeWitt, MD, FACG1, Jeffrey Easler, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2Mayo Clinic, Rochester, MN; 3Icahn School of Medicine at Mount Sinai, Queens, NY; 4Indiana University, Indianapolis, IN
Introduction: Gastric variceal (GV) bleeding can be treated with either direct endoscopic cyanoacrylate (CYA) glue injection therapy (DEG-T) and endoscopic ultrasound (EUS)-guided therapies (EUS-T), including CYA glue injection and/or coil embolization. The current data on the outcomes of EUS-T and DEG-T is largely based on a meta-analysis using indirect evidence from non-comparative studies. To provide more reliable insights, we conducted a meta-analysis of studies that directly compared EUS-T with DEG-T.
Methods: We searched PubMed, Embase, and Web of Science databases to include all comparative studies that assessed the outcomes of EUS-T with DEG-T for GV bleeding. Single-arm studies were excluded. Pooled mean difference (MD) and risk ratio (RR) with 95% confidence intervals (CIs) were obtained within a random-effect model.
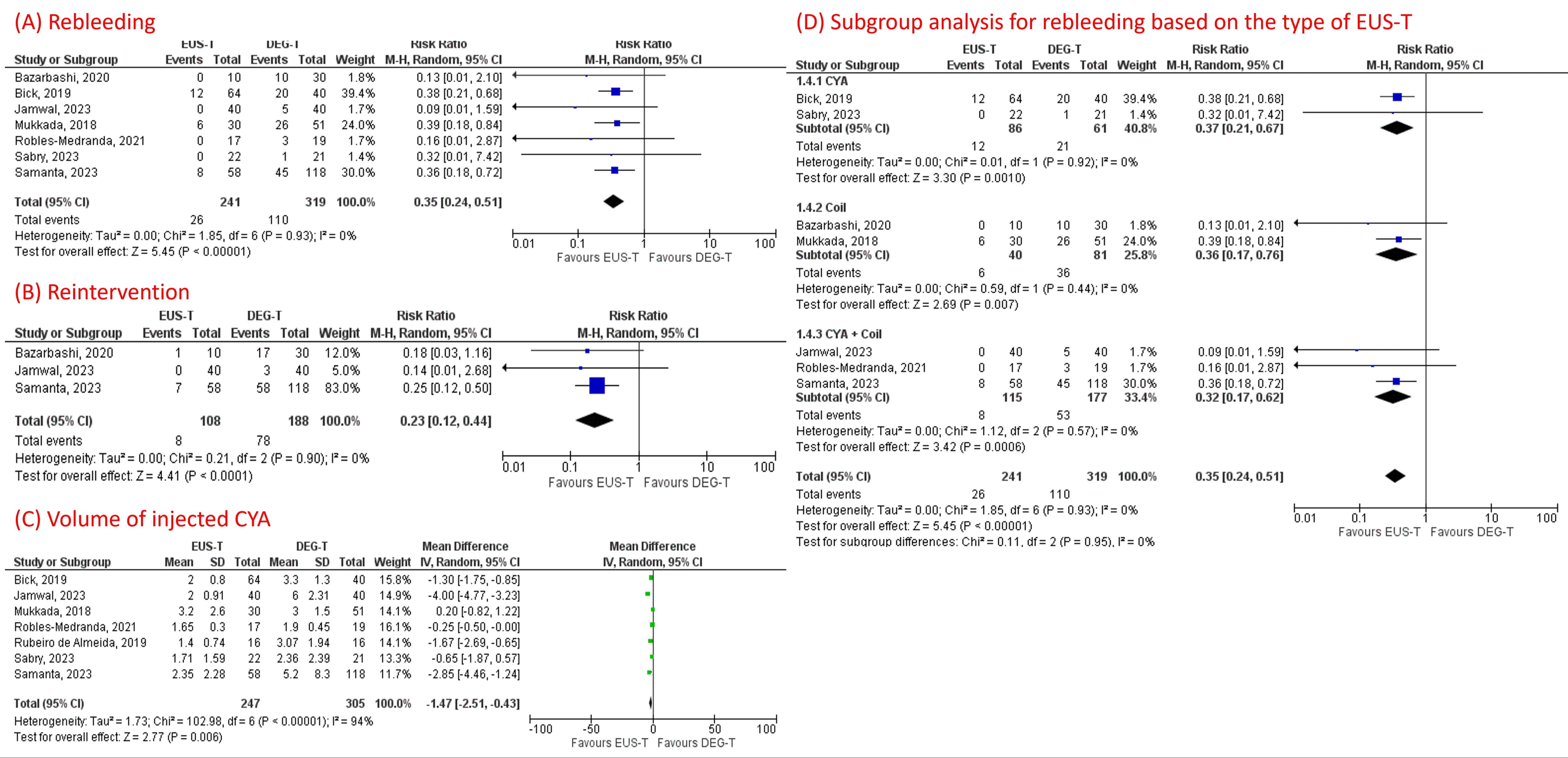
Results: Eight studies (six observational studies and two randomized controlled trials [RCT]) with 592 patients with GV (n=257 EUS-T vs. n=335 DEG-T) were included. EUS-T was associated with lower rebleeding (RR 0.35, 95% CI 0.24-0.51, p< 0.001), lower reintervention (RR 0.23, 95% CI 0.12-0.44, p< 0.001), and lower volume of CYA (MD -1.47 mL; 95% CI -2.51, -0.43; p=0.006) than DEG-T (Figure 1). Subgroup analysis for rebleeding based on the type of EUS-T showed consistent results favoring EUS-T over DEG-T regardless of whether patients received CYA injection (RR 0.37, 95% CI 0.21-0.67), coil embolization (RR 0.36, 95% CI 0.17-0.76) or combined CYA injection and coil embolization (RR 0.32, 95% CI 0.17-0.62) (Figure 1). There was a trend toward fewer treatment sessions (MD -0.32; 95% CI -0.67, 0.03; p=0.07), fewer overall complications (RR 0.53, 95% CI 0.24-1.17, p=0.12), and lower rates of pulmonary embolism (RR 0.54, 95% CI 0.23-1.27, p=0.16) with EUS-T compared to DEG-T but did not reach statistical significance. There was no significant difference in technical success (RR 1.03, 95% CI 0.93-1.14, p=0.57) and all-cause mortality (RR 0.93, 95% CI 0.23-3.73, p=0.92) between the two groups.
Discussion: EUS-guided therapy technique for GV bleeding was associated with lower rates of rebleeding and reintervention and comparable rates of complications compared to direct endoscopic glue injection. Moreover, EUS-guided therapy required a lower volume of CYA injection. Our data suggests an EUS-guided technique is a more effective option for treating GV bleeding. More RCTs are needed to evaluate the interval benefit of an EUS-guided approach.
Disclosures:
Azizullah Beran, MD1, Mouhand F.H. Mohamed, MD, MSc2, Hazem Abosheaishaa, MD3, Hala Fatima, MD4, Mark A. Gromski, MD1, Mohammad Al-Haddad, MD, FACG1, John M. DeWitt, MD, FACG1, Jeffrey Easler, MD1. P2783 - Comparative Effectiveness and Safety of Endoscopic Ultrasound-Guided Therapy versus Direct Endoscopic Glue Injection Therapy for Gastric Varices: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Mayo Clinic, Rochester, MN; 3Icahn School of Medicine at Mount Sinai, Queens, NY; 4Indiana University, Indianapolis, IN
Introduction: Gastric variceal (GV) bleeding can be treated with either direct endoscopic cyanoacrylate (CYA) glue injection therapy (DEG-T) and endoscopic ultrasound (EUS)-guided therapies (EUS-T), including CYA glue injection and/or coil embolization. The current data on the outcomes of EUS-T and DEG-T is largely based on a meta-analysis using indirect evidence from non-comparative studies. To provide more reliable insights, we conducted a meta-analysis of studies that directly compared EUS-T with DEG-T.
Methods: We searched PubMed, Embase, and Web of Science databases to include all comparative studies that assessed the outcomes of EUS-T with DEG-T for GV bleeding. Single-arm studies were excluded. Pooled mean difference (MD) and risk ratio (RR) with 95% confidence intervals (CIs) were obtained within a random-effect model.
Results: Eight studies (six observational studies and two randomized controlled trials [RCT]) with 592 patients with GV (n=257 EUS-T vs. n=335 DEG-T) were included. EUS-T was associated with lower rebleeding (RR 0.35, 95% CI 0.24-0.51, p< 0.001), lower reintervention (RR 0.23, 95% CI 0.12-0.44, p< 0.001), and lower volume of CYA (MD -1.47 mL; 95% CI -2.51, -0.43; p=0.006) than DEG-T (Figure 1). Subgroup analysis for rebleeding based on the type of EUS-T showed consistent results favoring EUS-T over DEG-T regardless of whether patients received CYA injection (RR 0.37, 95% CI 0.21-0.67), coil embolization (RR 0.36, 95% CI 0.17-0.76) or combined CYA injection and coil embolization (RR 0.32, 95% CI 0.17-0.62) (Figure 1). There was a trend toward fewer treatment sessions (MD -0.32; 95% CI -0.67, 0.03; p=0.07), fewer overall complications (RR 0.53, 95% CI 0.24-1.17, p=0.12), and lower rates of pulmonary embolism (RR 0.54, 95% CI 0.23-1.27, p=0.16) with EUS-T compared to DEG-T but did not reach statistical significance. There was no significant difference in technical success (RR 1.03, 95% CI 0.93-1.14, p=0.57) and all-cause mortality (RR 0.93, 95% CI 0.23-3.73, p=0.92) between the two groups.
Discussion: EUS-guided therapy technique for GV bleeding was associated with lower rates of rebleeding and reintervention and comparable rates of complications compared to direct endoscopic glue injection. Moreover, EUS-guided therapy required a lower volume of CYA injection. Our data suggests an EUS-guided technique is a more effective option for treating GV bleeding. More RCTs are needed to evaluate the interval benefit of an EUS-guided approach.
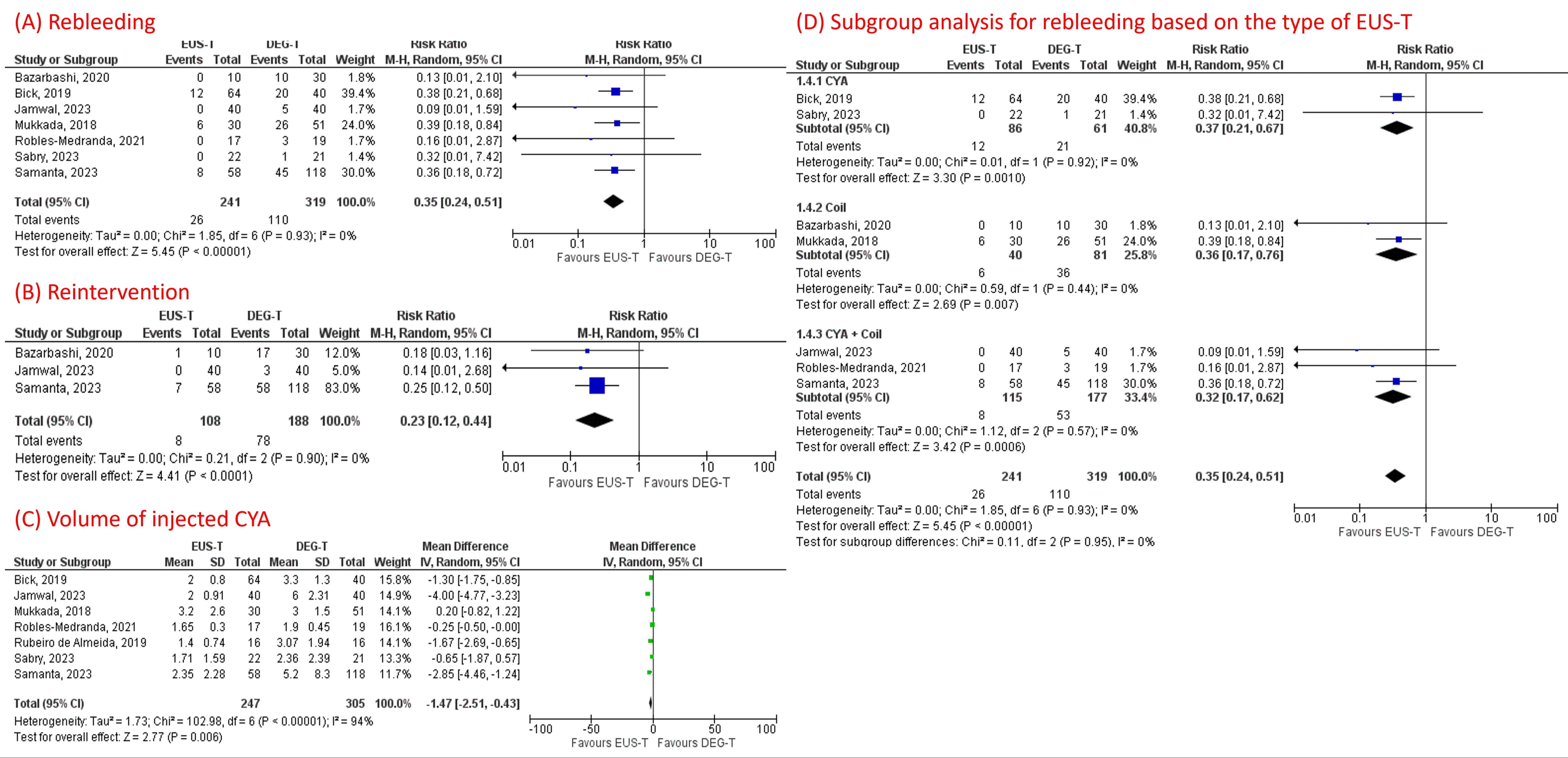
Figure: Figure 1
Disclosures:
Azizullah Beran indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Hala Fatima indicated no relevant financial relationships.
Mark Gromski: Allurion – Grant/Research Support. Ambu – Consultant. Boston Scientific – Consultant. Cook Medical – Grant/Research Support. Fractyl – Grant/Research Support.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace Diagnostics – Consultant.
John DeWitt indicated no relevant financial relationships.
Jeffrey Easler: Boston Scientific – Consultant.
Azizullah Beran, MD1, Mouhand F.H. Mohamed, MD, MSc2, Hazem Abosheaishaa, MD3, Hala Fatima, MD4, Mark A. Gromski, MD1, Mohammad Al-Haddad, MD, FACG1, John M. DeWitt, MD, FACG1, Jeffrey Easler, MD1. P2783 - Comparative Effectiveness and Safety of Endoscopic Ultrasound-Guided Therapy versus Direct Endoscopic Glue Injection Therapy for Gastric Varices: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
