Monday Poster Session
Category: IBD
P2695 - The Great Mimicker: Intestinal Tuberculosis Disguising Itself as Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Vera Hapshy, DO
Jersey Shore University Medical Center
Marlboro, NJ
Presenting Author(s)
Vera Hapshy, DO1, Anne Marie Arcidiacono, DO2, Lauren Klei, MD2, Harshavardan Sannekommu, MD2, Hannah Cantwell, BA2, Alexandra Berezan, BA2, Steven Imburgio, MD2, Swapnil Patel, MD2, Mohammad Hossain, MD2, Lee Peng, MD, PhD3
1Jersey Shore University Medical Center, Marlboro, NJ; 2Jersey Shore University Medical Center, Neptune, NJ; 3Jersey Shore University Medical Center, Neptune City, NJ
Introduction: Gastrointestinal manifestations of tuberculosis (TB) often mimic symptoms of inflammatory bowel disease (IBD), leading to potential misdiagnosis. Here we present a rare case of intestinal tuberculous ileotyphlitis initially mistaken for Crohn’s disease.
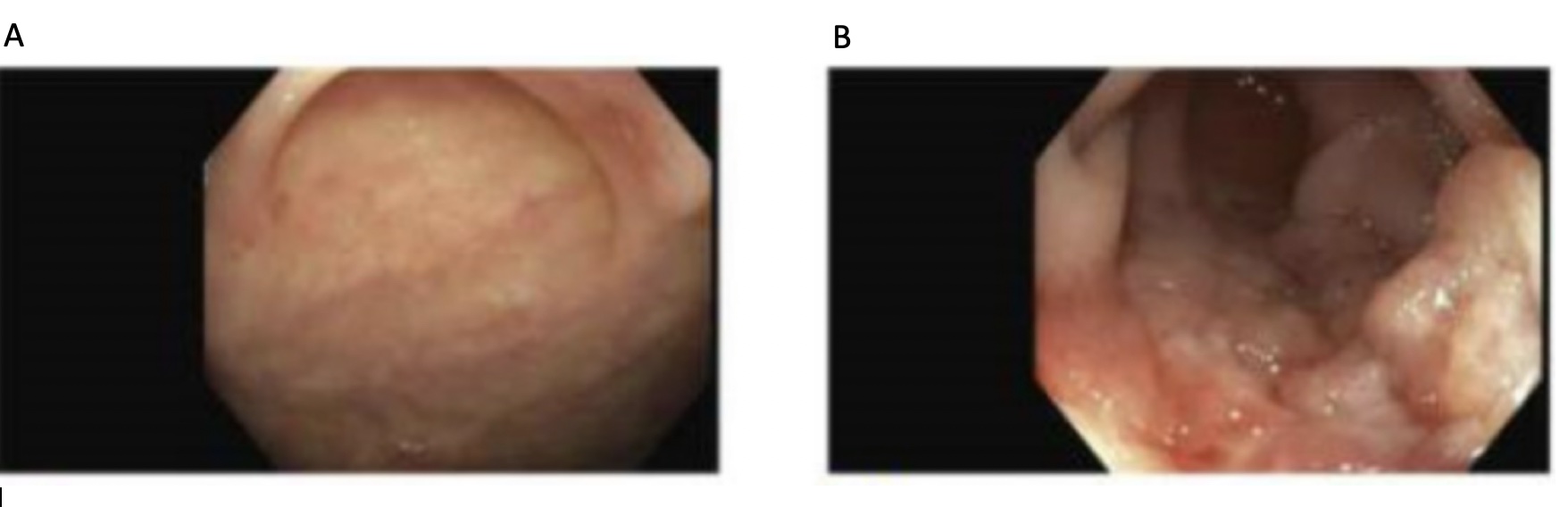
Case Description/Methods: A 25-year-old female immigrant from Honduras with no reported medical history presented with chronic abdominal pain, vomiting, and significant weight loss. She was hypotensive and cachectic. Lab studies indicated elevated inflammatory markers with initial imaging negative. An EGD revealed antral gastritis with H. pylori, and colonoscopy showed terminal ileum ulcerations with small ulcers at the appendiceal orifice and transverse colon - leading to a high suspicion of Crohn’s disease (Figure 1). TB testing was sent as a precaution for biologic therapy preparation. Days later, acid-fast bacilli (AFB) smear from stool and sputum tested positive for TB. She was diagnosed with tuberculous ileotyphlitis and started on RIPE therapy. Pathology showed ileal acute inflammation with chronic inflammation, but no AFB organisms. The patient continued RIPE therapy for 14 days and was discharged with plans for a follow-up colonoscopy.
Discussion: Intestinal TB and Crohn’s disease share clinical, radiologic, and histologic features, complicating diagnosis with no single test confirming either disease. Intestinal TB progresses more insidiously than Crohn’s, unless complicated by obstruction, perforation, or fistula formation. Both conditions manifest with fever, night sweats, and extraintestinal involvement. On colonoscopy, intestinal TB can present with ulcerations, polyps, or hypertrophic changes, resulting in strictures with fistulae. Crohn’s disease can show similar findings but typically includes skip lesions and pseudopolyps. Additionally, both diseases primarily affect the terminal ileum with transmural inflammation and histologically, TB shows caseating necrotic granulomas, while Crohn’s shows non-caseating granulomas. Our patient had terminal ileum ulcerations and inflammation with no AFB on biopsies but positive AFB stool cultures, consistent with tuberculous ileotyphlitis. Differentiating these diseases is crucial as TB treatment requires RIPE therapy, while Crohn’s treatment involves corticosteroids, immunosuppressants, and possibly biologics, which can reactivate or worsen TB. Extra-pulmonary TB is often underdiagnosed and mimics IBD, necessitating careful consideration to ensure timely treatment.
Disclosures:
Vera Hapshy, DO1, Anne Marie Arcidiacono, DO2, Lauren Klei, MD2, Harshavardan Sannekommu, MD2, Hannah Cantwell, BA2, Alexandra Berezan, BA2, Steven Imburgio, MD2, Swapnil Patel, MD2, Mohammad Hossain, MD2, Lee Peng, MD, PhD3. P2695 - The Great Mimicker: Intestinal Tuberculosis Disguising Itself as Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jersey Shore University Medical Center, Marlboro, NJ; 2Jersey Shore University Medical Center, Neptune, NJ; 3Jersey Shore University Medical Center, Neptune City, NJ
Introduction: Gastrointestinal manifestations of tuberculosis (TB) often mimic symptoms of inflammatory bowel disease (IBD), leading to potential misdiagnosis. Here we present a rare case of intestinal tuberculous ileotyphlitis initially mistaken for Crohn’s disease.
Case Description/Methods: A 25-year-old female immigrant from Honduras with no reported medical history presented with chronic abdominal pain, vomiting, and significant weight loss. She was hypotensive and cachectic. Lab studies indicated elevated inflammatory markers with initial imaging negative. An EGD revealed antral gastritis with H. pylori, and colonoscopy showed terminal ileum ulcerations with small ulcers at the appendiceal orifice and transverse colon - leading to a high suspicion of Crohn’s disease (Figure 1). TB testing was sent as a precaution for biologic therapy preparation. Days later, acid-fast bacilli (AFB) smear from stool and sputum tested positive for TB. She was diagnosed with tuberculous ileotyphlitis and started on RIPE therapy. Pathology showed ileal acute inflammation with chronic inflammation, but no AFB organisms. The patient continued RIPE therapy for 14 days and was discharged with plans for a follow-up colonoscopy.
Discussion: Intestinal TB and Crohn’s disease share clinical, radiologic, and histologic features, complicating diagnosis with no single test confirming either disease. Intestinal TB progresses more insidiously than Crohn’s, unless complicated by obstruction, perforation, or fistula formation. Both conditions manifest with fever, night sweats, and extraintestinal involvement. On colonoscopy, intestinal TB can present with ulcerations, polyps, or hypertrophic changes, resulting in strictures with fistulae. Crohn’s disease can show similar findings but typically includes skip lesions and pseudopolyps. Additionally, both diseases primarily affect the terminal ileum with transmural inflammation and histologically, TB shows caseating necrotic granulomas, while Crohn’s shows non-caseating granulomas. Our patient had terminal ileum ulcerations and inflammation with no AFB on biopsies but positive AFB stool cultures, consistent with tuberculous ileotyphlitis. Differentiating these diseases is crucial as TB treatment requires RIPE therapy, while Crohn’s treatment involves corticosteroids, immunosuppressants, and possibly biologics, which can reactivate or worsen TB. Extra-pulmonary TB is often underdiagnosed and mimics IBD, necessitating careful consideration to ensure timely treatment.
Figure: Figure 1: Colonoscopy images. A. Shallow ulcer in the Appendiceal Orifice. B. Edematous and ulcerated mucosa in the terminal ileum.
Disclosures:
Vera Hapshy indicated no relevant financial relationships.
Anne Marie Arcidiacono indicated no relevant financial relationships.
Lauren Klei indicated no relevant financial relationships.
Harshavardan Sannekommu indicated no relevant financial relationships.
Hannah Cantwell indicated no relevant financial relationships.
Alexandra Berezan indicated no relevant financial relationships.
Steven Imburgio indicated no relevant financial relationships.
Swapnil Patel indicated no relevant financial relationships.
Mohammad Hossain indicated no relevant financial relationships.
Lee Peng indicated no relevant financial relationships.
Vera Hapshy, DO1, Anne Marie Arcidiacono, DO2, Lauren Klei, MD2, Harshavardan Sannekommu, MD2, Hannah Cantwell, BA2, Alexandra Berezan, BA2, Steven Imburgio, MD2, Swapnil Patel, MD2, Mohammad Hossain, MD2, Lee Peng, MD, PhD3. P2695 - The Great Mimicker: Intestinal Tuberculosis Disguising Itself as Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

