Monday Poster Session
Category: IBD
P2698 - Visceral Kaposi Sarcoma in a Critically Ill Patient With Ulcerative Colitis and History of Liver Transplant
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zachary Makovich, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Zachary Makovich, MD1, Susan Jacob, MD2, Michael Daniel, MD1
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL
Introduction: Kaposi sarcoma (KS) is a soft tissue vascular tumor associated with Human Herpesvirus 8 (HHV-8). Prior estimation of KS incidence in liver transplant patients is around 2.1%.[1] Rarely, gastrointestinal KS may mimic treatment-refractory ulcerative colitis (UC). We present a case of visceral KS following liver transplant in a patient with UC and superimposed clostridium difficile infection (CDI).
Case Description/Methods: A 59-year-old male presented with 2-3 months of progressive non-bloody diarrhea. Pertinent history included UC and primary sclerosing cholangitis with liver transplant 6 months prior. His symptoms coincided with tapering his prednisone and tacrolimus used for liver transplant immunosuppression, but failed to improve after increasing prednisone. The patient was found to have CDI and initially improved with fidaxomicin, but then was subsequently re-admitted for bloody diarrhea.
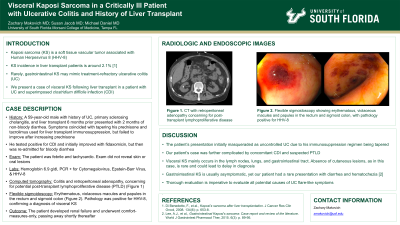
On re-admission, the patient was febrile and tachycardic. Exam did not reveal skin or oral lesions. Labs were notable for a hemoglobin of 6.9 g/dl. Polymerase chain reaction was positive for Cytomegalovirus, Epstein-Barr Virus, and HHV-8. Imaging showed colitis and retroperitoneal adenopathy, concerning for potential post-transplant lymphoproliferative disease (PTLD) (Figure 1a). Flexible sigmoidoscopy showed erythematous, violaceous macules and papules in the rectum and sigmoid colon (Figure 1b and 1c). Pathology was positive for HHV-8, confirming a diagnosis of visceral KS. The patient developed renal failure and underwent comfort-measures-only, passing away shortly thereafter.
Discussion: The patient’s presentation initially masqueraded as uncontrolled UC due to his immunosuppression regimen being tapered. Our patient’s case was further complicated by concomitant CDI and suspected PTLD. Visceral KS mainly occurs in the lymph nodes, lungs, and gastrointestinal tract. Absence of cutaneous lesions, as in this case, is rare and could lead to delay in diagnosis. In addition, gastrointestinal KS is usually asymptomatic, yet our patient had a rare presentation with diarrhea and hematochezia.[2] Thorough evaluation is imperative to evaluate all potential causes of UC flare-like symptoms.
References
1. Di Benedetto, F., et al., Kaposi's sarcoma after liver transplantation. J Cancer Res Clin Oncol, 2008. 134(6): p. 653-8.
2. Lee, A.J., et al., Gastrointestinal Kaposi's sarcoma: Case report and review of the literature. World J Gastrointest Pharmacol Ther, 2015. 6(3): p. 89-95.

Disclosures:
Zachary Makovich, MD1, Susan Jacob, MD2, Michael Daniel, MD1. P2698 - Visceral Kaposi Sarcoma in a Critically Ill Patient With Ulcerative Colitis and History of Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL
Introduction: Kaposi sarcoma (KS) is a soft tissue vascular tumor associated with Human Herpesvirus 8 (HHV-8). Prior estimation of KS incidence in liver transplant patients is around 2.1%.[1] Rarely, gastrointestinal KS may mimic treatment-refractory ulcerative colitis (UC). We present a case of visceral KS following liver transplant in a patient with UC and superimposed clostridium difficile infection (CDI).
Case Description/Methods: A 59-year-old male presented with 2-3 months of progressive non-bloody diarrhea. Pertinent history included UC and primary sclerosing cholangitis with liver transplant 6 months prior. His symptoms coincided with tapering his prednisone and tacrolimus used for liver transplant immunosuppression, but failed to improve after increasing prednisone. The patient was found to have CDI and initially improved with fidaxomicin, but then was subsequently re-admitted for bloody diarrhea.
On re-admission, the patient was febrile and tachycardic. Exam did not reveal skin or oral lesions. Labs were notable for a hemoglobin of 6.9 g/dl. Polymerase chain reaction was positive for Cytomegalovirus, Epstein-Barr Virus, and HHV-8. Imaging showed colitis and retroperitoneal adenopathy, concerning for potential post-transplant lymphoproliferative disease (PTLD) (Figure 1a). Flexible sigmoidoscopy showed erythematous, violaceous macules and papules in the rectum and sigmoid colon (Figure 1b and 1c). Pathology was positive for HHV-8, confirming a diagnosis of visceral KS. The patient developed renal failure and underwent comfort-measures-only, passing away shortly thereafter.
Discussion: The patient’s presentation initially masqueraded as uncontrolled UC due to his immunosuppression regimen being tapered. Our patient’s case was further complicated by concomitant CDI and suspected PTLD. Visceral KS mainly occurs in the lymph nodes, lungs, and gastrointestinal tract. Absence of cutaneous lesions, as in this case, is rare and could lead to delay in diagnosis. In addition, gastrointestinal KS is usually asymptomatic, yet our patient had a rare presentation with diarrhea and hematochezia.[2] Thorough evaluation is imperative to evaluate all potential causes of UC flare-like symptoms.
References
1. Di Benedetto, F., et al., Kaposi's sarcoma after liver transplantation. J Cancer Res Clin Oncol, 2008. 134(6): p. 653-8.
2. Lee, A.J., et al., Gastrointestinal Kaposi's sarcoma: Case report and review of the literature. World J Gastrointest Pharmacol Ther, 2015. 6(3): p. 89-95.

Figure: Figure 1. Computed tomography demonstrated retroperitoneal and para-aortic adenopathy (A). Flexible sigmoidoscopy revealed violaceous macules and papules in the rectum and sigmoid colon (B,C).
Disclosures:
Zachary Makovich indicated no relevant financial relationships.
Susan Jacob indicated no relevant financial relationships.
Michael Daniel indicated no relevant financial relationships.
Zachary Makovich, MD1, Susan Jacob, MD2, Michael Daniel, MD1. P2698 - Visceral Kaposi Sarcoma in a Critically Ill Patient With Ulcerative Colitis and History of Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
