Monday Poster Session
Category: IBD
P2703 - Using a Smartwatch as a Diagnostic Tool in a Patient with Ulcerative Colitis who Developed Unexplained Anemia and Hypoxia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- TM
Thomas J. Mathews, MD
University of Kansas Medical Center
Kansas City, MO
Presenting Author(s)
Thomas J.. Mathews, MD1, Anthony Mok, MD1, Mollie Jackson, DO2
1University of Kansas Medical Center, Kansas City, MO; 2University of Kansas Medical Center, Kansas City, KS
Introduction: Methemoglobinemia is a relatively uncommon cause of hypoxia in patients but should be suspected in patients with unexplained cyanosis or hypoxia that does not improve with supplemental oxygen, especially when taking medication with the known side effect. In this case, our patient was told her new anemia and hypoxia was from her ulcerative colitis (UC) despite her reporting no bleeding. Further, her smartwatch was able to aid in the diagnosis of methemoglobinemia.
Case Description/Methods: 38-year-old female with UC on vedolizumab, prednisone, and recently started upadacitinib presented to the emergency department (ED) with hypoxia. Patient was a physician and noticed her smartwatch was notifying her of low oxygen saturations ~88% for the past week. She was otherwise asymptomatic with no dyspnea, chest pain, cough, or fever.
She recently started upadacitinib 10 days ago. Prior to initiation, her UC was so severe that she had not been able to work for a month prior; however, within 36 hours of initiation, her symptoms had greatly improved, and she was no longer having diarrhea, abdominal pain, or hematochezia. Given her medical knowledge, she was concerned for a blood clot or pulmonary embolism (PE) in the setting of her recently started upadacitinib as the cause of her hypoxia.
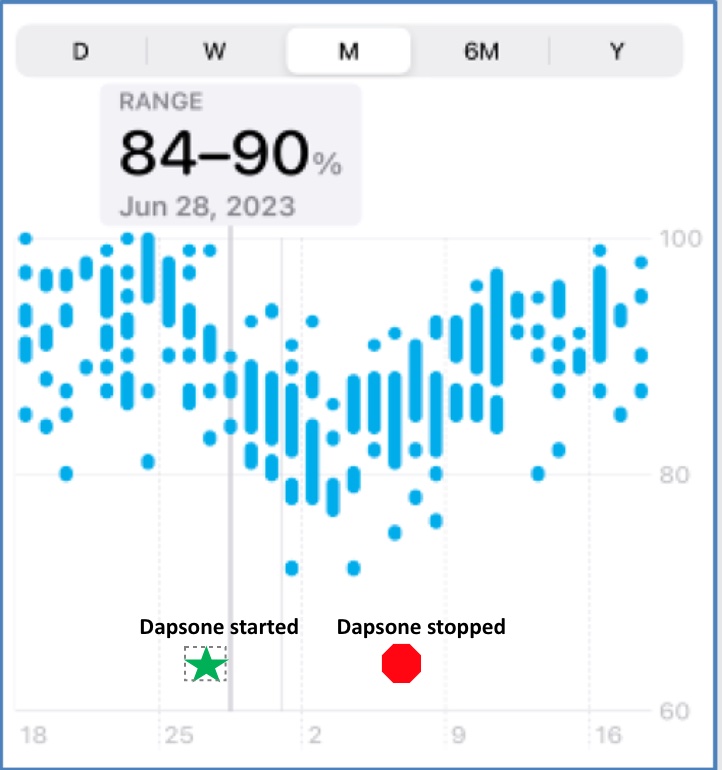
In the ED, she was started on 3 liters of O2 without improvement in oxygen levels. CTA chest was negative for PE or consolidation. TTE, RVP, BNP, troponin, and procalcitonin were unremarkable. Her Hemoglobin (Hgb) was low at 9 (baseline ~13) despite no hematochezia or bleeding. Upon further investigation, it was found that she started dapsone 3 days after her upadacitinib initiation. Her desaturation notifications on her smart watch began promptly the following day (figure 1). Methemoglobin level was significantly elevated at 11.4% and ABG showed an O2 saturation of 99% despite oximetry reading 89%. Dapsone was discontinued and switched to pentamidine. One month later, she remained in clinical remission with no recurrent episodes of hypoxia and Hgb improved back to baseline.
Discussion: This case emphasizes the importance of a detailed history. Initially, her anemia was attributed to her UC and blood loss. However, it was revealed that she no longer had hematochezia and was started on new medication. Additionally, advancement in smartwatch technology helped prompt her to seek medical attention and correlate timing of symptoms for a quick diagnosis, allowing her to be properly treated by removing the offending agent.
Disclosures:
Thomas J.. Mathews, MD1, Anthony Mok, MD1, Mollie Jackson, DO2. P2703 - Using a Smartwatch as a Diagnostic Tool in a Patient with Ulcerative Colitis who Developed Unexplained Anemia and Hypoxia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas Medical Center, Kansas City, MO; 2University of Kansas Medical Center, Kansas City, KS
Introduction: Methemoglobinemia is a relatively uncommon cause of hypoxia in patients but should be suspected in patients with unexplained cyanosis or hypoxia that does not improve with supplemental oxygen, especially when taking medication with the known side effect. In this case, our patient was told her new anemia and hypoxia was from her ulcerative colitis (UC) despite her reporting no bleeding. Further, her smartwatch was able to aid in the diagnosis of methemoglobinemia.
Case Description/Methods: 38-year-old female with UC on vedolizumab, prednisone, and recently started upadacitinib presented to the emergency department (ED) with hypoxia. Patient was a physician and noticed her smartwatch was notifying her of low oxygen saturations ~88% for the past week. She was otherwise asymptomatic with no dyspnea, chest pain, cough, or fever.
She recently started upadacitinib 10 days ago. Prior to initiation, her UC was so severe that she had not been able to work for a month prior; however, within 36 hours of initiation, her symptoms had greatly improved, and she was no longer having diarrhea, abdominal pain, or hematochezia. Given her medical knowledge, she was concerned for a blood clot or pulmonary embolism (PE) in the setting of her recently started upadacitinib as the cause of her hypoxia.
In the ED, she was started on 3 liters of O2 without improvement in oxygen levels. CTA chest was negative for PE or consolidation. TTE, RVP, BNP, troponin, and procalcitonin were unremarkable. Her Hemoglobin (Hgb) was low at 9 (baseline ~13) despite no hematochezia or bleeding. Upon further investigation, it was found that she started dapsone 3 days after her upadacitinib initiation. Her desaturation notifications on her smart watch began promptly the following day (figure 1). Methemoglobin level was significantly elevated at 11.4% and ABG showed an O2 saturation of 99% despite oximetry reading 89%. Dapsone was discontinued and switched to pentamidine. One month later, she remained in clinical remission with no recurrent episodes of hypoxia and Hgb improved back to baseline.
Discussion: This case emphasizes the importance of a detailed history. Initially, her anemia was attributed to her UC and blood loss. However, it was revealed that she no longer had hematochezia and was started on new medication. Additionally, advancement in smartwatch technology helped prompt her to seek medical attention and correlate timing of symptoms for a quick diagnosis, allowing her to be properly treated by removing the offending agent.
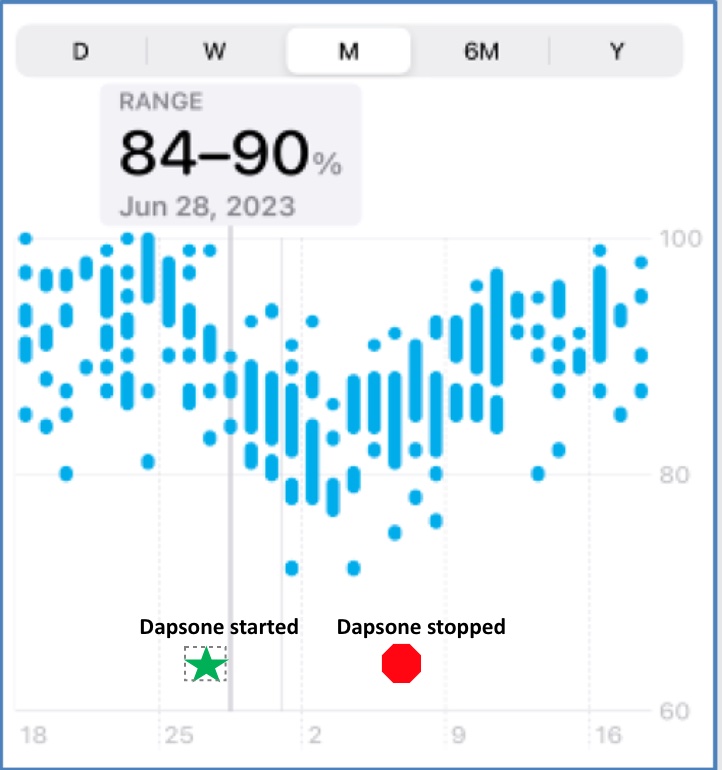
Figure: Smartwatch Oxygen Saturation Readings Before and After Starting Dapsone
Disclosures:
Thomas Mathews indicated no relevant financial relationships.
Anthony Mok indicated no relevant financial relationships.
Mollie Jackson indicated no relevant financial relationships.
Thomas J.. Mathews, MD1, Anthony Mok, MD1, Mollie Jackson, DO2. P2703 - Using a Smartwatch as a Diagnostic Tool in a Patient with Ulcerative Colitis who Developed Unexplained Anemia and Hypoxia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
