Monday Poster Session
Category: IBD
P2609 - Impact of Sociodemographic Status on Hospital Length of Stay in Inflammatory Bowel Disease (IBD) Patients
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Carla Barberan Parraga, MD
Maimonides Medical Center
New York, NY
Presenting Author(s)
Carla Barberan Parraga, MD1, Kundan Jana, MBBS2, Leandro Sierra, MD3, Samantha S. Ehrlich, MD, MPH2, Nazli Begum Ozturk, MD4, Ahmed E. Salem, MBBCh2, Michael Kantrowitz, DO, MS2
1Maimonides Medical Center, New York, NY; 2Maimonides Medical Center, Brooklyn, NY; 3Cleveland Clinic Foundation, Cleveland, OH; 4Corewell Health William Beaumont University Hospital, Royal Oak, MI
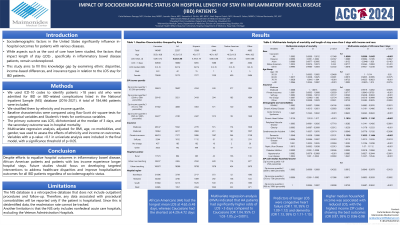
Introduction: Sociodemographic factors significantly influence in-hospital outcomes for patients in the United States. While cost of care is studied, factors impacting length of stay (LOS) in inflammatory bowel disease (IBD) patients are underexplored. This study aims to fill this gap by examining ethnic disparities, income differences, and insurance types in relation to the LOS stay for IBD patients.
Methods: Patients >18 years old with an IBD-related admission (2016-2021) were identified from the National Inpatient Sample (NIS) database using ICD-10 codes. They were stratified by ethnicity and income quartile. Baseline characteristics were compared using appropriate tests. The primary outcome was LOS, dichotomized at the median of 3 days, and the secondary outcome was in-hospital mortality. Multivariate regression was adjusted for BMI, age, co-morbidities, and gender, and the effects of ethnicity and income on outcomes were analyzed. Variables with a p-value < 0.1 in univariate analysis were included in the final model, with a significance of p < 0.05. Data extraction was conducted with Python (version 3.9.1), and analysis was performed using the survey package in R (version 3.6.2).
Results: 184,446 patients of diverse ethnic backgrounds were included in the study. African Americans (AA) had the longest mean LOS at 4.62±5.48 days, whereas Caucasians had the shortest at 4.29±4.72 days. Multivariate regression analysis (MVA) indicated that AA had significantly higher odds of LOS >3 days vs. Caucasians (OR 1.04, 95% CI 1.03-1.05, p< 0.001). Predictors of reduced LOS included self-payment (OR 0.96, 95% CI 0.94-0.97, p< 0.001), female gender (OR 0.99, 95% CI 0.98-0.99, p< 0.001), and acute coronary syndrome (ACS) as a comorbidity (OR 0.87, 95% CI 0.85-0.88, p< 0.001). Conversely, predictors of longer LOS were congestive heart failure (OR 1.10, 95% CI 1.09-1.12) and dementia (OR 1.13, 95% CI 1.11-1.15). Income analysis showed that higher median household income was associated with reduced LOS, with the highest income ZIP codes showing the best outcomes (OR 0.97, 95% CI 0.96-0.98). However, income did not demonstrate a significant association with mortality.
Discussion: Despite efforts to equalize outcomes in IBD, African American patients and low-income patients experience longer hospital stays. Future studies should focus on developing targeted interventions to address healthcare disparities and improve hospitalization outcomes for all IBD patients regardless of sociodemographic status.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carla Barberan Parraga, MD1, Kundan Jana, MBBS2, Leandro Sierra, MD3, Samantha S. Ehrlich, MD, MPH2, Nazli Begum Ozturk, MD4, Ahmed E. Salem, MBBCh2, Michael Kantrowitz, DO, MS2. P2609 - Impact of Sociodemographic Status on Hospital Length of Stay in Inflammatory Bowel Disease (IBD) Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Maimonides Medical Center, New York, NY; 2Maimonides Medical Center, Brooklyn, NY; 3Cleveland Clinic Foundation, Cleveland, OH; 4Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Sociodemographic factors significantly influence in-hospital outcomes for patients in the United States. While cost of care is studied, factors impacting length of stay (LOS) in inflammatory bowel disease (IBD) patients are underexplored. This study aims to fill this gap by examining ethnic disparities, income differences, and insurance types in relation to the LOS stay for IBD patients.
Methods: Patients >18 years old with an IBD-related admission (2016-2021) were identified from the National Inpatient Sample (NIS) database using ICD-10 codes. They were stratified by ethnicity and income quartile. Baseline characteristics were compared using appropriate tests. The primary outcome was LOS, dichotomized at the median of 3 days, and the secondary outcome was in-hospital mortality. Multivariate regression was adjusted for BMI, age, co-morbidities, and gender, and the effects of ethnicity and income on outcomes were analyzed. Variables with a p-value < 0.1 in univariate analysis were included in the final model, with a significance of p < 0.05. Data extraction was conducted with Python (version 3.9.1), and analysis was performed using the survey package in R (version 3.6.2).
Results: 184,446 patients of diverse ethnic backgrounds were included in the study. African Americans (AA) had the longest mean LOS at 4.62±5.48 days, whereas Caucasians had the shortest at 4.29±4.72 days. Multivariate regression analysis (MVA) indicated that AA had significantly higher odds of LOS >3 days vs. Caucasians (OR 1.04, 95% CI 1.03-1.05, p< 0.001). Predictors of reduced LOS included self-payment (OR 0.96, 95% CI 0.94-0.97, p< 0.001), female gender (OR 0.99, 95% CI 0.98-0.99, p< 0.001), and acute coronary syndrome (ACS) as a comorbidity (OR 0.87, 95% CI 0.85-0.88, p< 0.001). Conversely, predictors of longer LOS were congestive heart failure (OR 1.10, 95% CI 1.09-1.12) and dementia (OR 1.13, 95% CI 1.11-1.15). Income analysis showed that higher median household income was associated with reduced LOS, with the highest income ZIP codes showing the best outcomes (OR 0.97, 95% CI 0.96-0.98). However, income did not demonstrate a significant association with mortality.
Discussion: Despite efforts to equalize outcomes in IBD, African American patients and low-income patients experience longer hospital stays. Future studies should focus on developing targeted interventions to address healthcare disparities and improve hospitalization outcomes for all IBD patients regardless of sociodemographic status.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carla Barberan Parraga indicated no relevant financial relationships.
Kundan Jana indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Samantha Ehrlich indicated no relevant financial relationships.
Nazli Begum Ozturk indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Michael Kantrowitz indicated no relevant financial relationships.
Carla Barberan Parraga, MD1, Kundan Jana, MBBS2, Leandro Sierra, MD3, Samantha S. Ehrlich, MD, MPH2, Nazli Begum Ozturk, MD4, Ahmed E. Salem, MBBCh2, Michael Kantrowitz, DO, MS2. P2609 - Impact of Sociodemographic Status on Hospital Length of Stay in Inflammatory Bowel Disease (IBD) Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
