Monday Poster Session
Category: IBD
P2617 - No Differences in Dysplasia Detection Between Dye and Virtual Chromoendoscopy Techniques: Results From a Meta-Analysis of Randomized Clinical Trials
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mouhand F.H Mohamed, MD, MSc
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mouhand F.H. Mohamed, MD, MSc1, Azizullah Beran, MD2, Khalid Ahmed, MD3, Samir A. Shah, MD4
1Mayo Clinic, Rochester, MN; 2Indiana University School of Medicine, Indianapolis, IN; 3University of Pennsylvania, Philadelphia, PA; 4Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI
Introduction: A recent meta-analysis revealed the superiority of dye chromoendoscopy (DCE) to high-definition (HD) white light endoscopy for dysplasia detection in inflammatory bowel disease (IBD) patients. This meta-analysis assesses dysplasia detection by HD scopes comparing DCE to virtual chromoendoscopy (VCE).
Methods: We comprehensively searched multiple databases (PubMed, EMBASE, and Cochrane Library) through March 2024. We limited our inclusion to randomized controlled trials (RCTs) utilizing HD scopes and comparing DCE and VCE (narrow band imaging [NBI], iSCAN, auto-fluorescence imaging [AFI], or flexible spectral imaging color enhancement [FICE]). The primary outcome was dysplasia detection, defined as the number of patients with at least one dysplastic lesion detected (this included adenomatous lesions). A comparativeness effectiveness meta-analysis utilizing the random effects model was performed. We used odds ratios (OR) for comparison with 95% confidence intervals (CI). I2 was used to assess heterogeneity. We did a subgroup analysis excluding AFI, a VCE technique deemed inferior to DCE by a multicentric RCT.
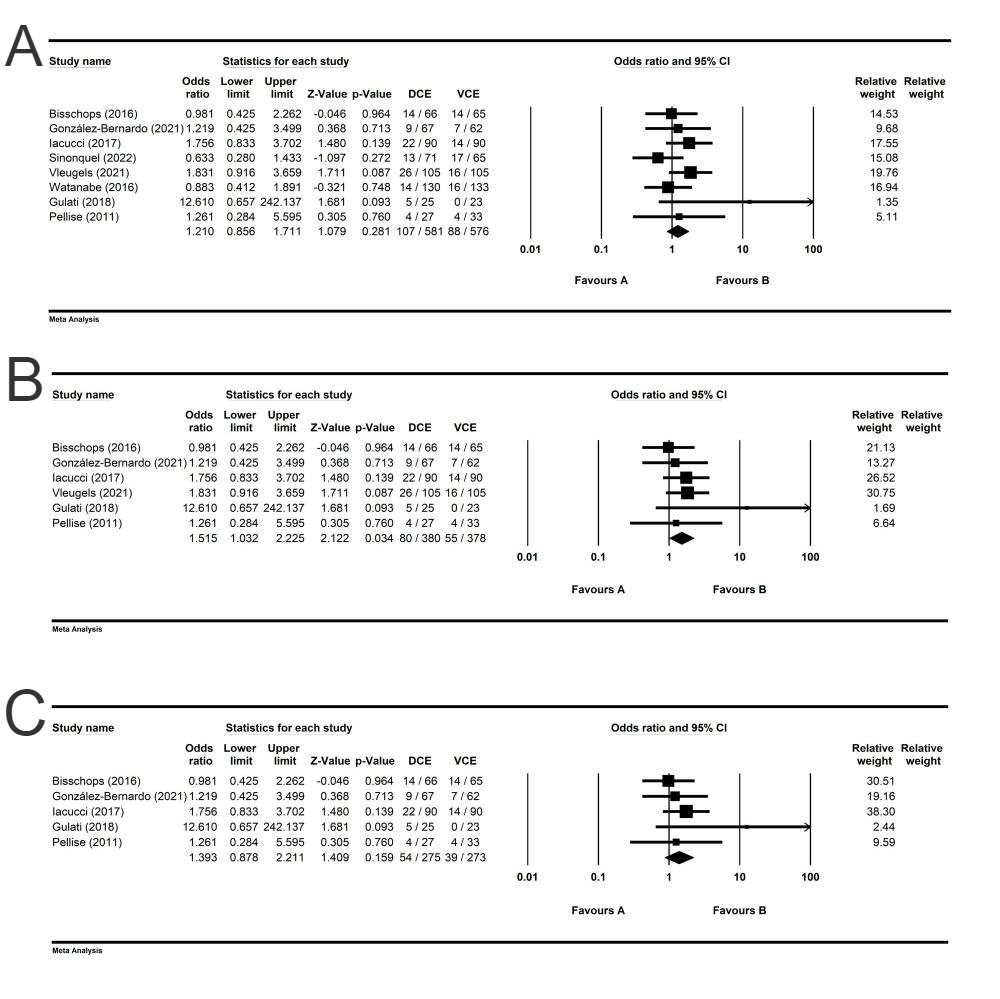
Results: Eight studies met our inclusion criteria and were included in the analysis. Six studies were published as full papers. Three RCTs used NBI, three used iSCAN, one used FICE, and one used AFI (Table 1). Overall, the dysplasia detection was not significantly different between DCE and VCE, OR 1.2 (95% CI 0.85-1.7, p=0.2, I2 13%) (Figure 1). An analysis limited to full-text articles, including six studies, showed higher dysplasia detection associated with DCE, OR 1.5 (95% CI 1.03-2.22 p=0.3, I2 0%)(Figure 1). Upon excluding one study evaluating AFI, no difference between DCE and VCE remained, OR 1.39 (95% CI 0.087-2.21 p=0.15, I2 0%) (Figure 1).
Discussion: This updated meta-analysis of RCTs utilizing HD scopes showed no significant differences in dysplasia detection between DCE and VCE, making VCE a viable alternative to DCE when DCE is not available. Based on a subgroup analysis including AFI, significantly higher dysplasia was detected via DCE. Thus, the results of this meta-analysis do not support AFI as an alternative to DCE in dysplasia detection in IBD. Further research is needed into the long-term outcomes of various screening modalities, including cancer and cancer-related death.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mouhand F.H. Mohamed, MD, MSc1, Azizullah Beran, MD2, Khalid Ahmed, MD3, Samir A. Shah, MD4. P2617 - No Differences in Dysplasia Detection Between Dye and Virtual Chromoendoscopy Techniques: Results From a Meta-Analysis of Randomized Clinical Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Indiana University School of Medicine, Indianapolis, IN; 3University of Pennsylvania, Philadelphia, PA; 4Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI
Introduction: A recent meta-analysis revealed the superiority of dye chromoendoscopy (DCE) to high-definition (HD) white light endoscopy for dysplasia detection in inflammatory bowel disease (IBD) patients. This meta-analysis assesses dysplasia detection by HD scopes comparing DCE to virtual chromoendoscopy (VCE).
Methods: We comprehensively searched multiple databases (PubMed, EMBASE, and Cochrane Library) through March 2024. We limited our inclusion to randomized controlled trials (RCTs) utilizing HD scopes and comparing DCE and VCE (narrow band imaging [NBI], iSCAN, auto-fluorescence imaging [AFI], or flexible spectral imaging color enhancement [FICE]). The primary outcome was dysplasia detection, defined as the number of patients with at least one dysplastic lesion detected (this included adenomatous lesions). A comparativeness effectiveness meta-analysis utilizing the random effects model was performed. We used odds ratios (OR) for comparison with 95% confidence intervals (CI). I2 was used to assess heterogeneity. We did a subgroup analysis excluding AFI, a VCE technique deemed inferior to DCE by a multicentric RCT.
Results: Eight studies met our inclusion criteria and were included in the analysis. Six studies were published as full papers. Three RCTs used NBI, three used iSCAN, one used FICE, and one used AFI (Table 1). Overall, the dysplasia detection was not significantly different between DCE and VCE, OR 1.2 (95% CI 0.85-1.7, p=0.2, I2 13%) (Figure 1). An analysis limited to full-text articles, including six studies, showed higher dysplasia detection associated with DCE, OR 1.5 (95% CI 1.03-2.22 p=0.3, I2 0%)(Figure 1). Upon excluding one study evaluating AFI, no difference between DCE and VCE remained, OR 1.39 (95% CI 0.087-2.21 p=0.15, I2 0%) (Figure 1).
Discussion: This updated meta-analysis of RCTs utilizing HD scopes showed no significant differences in dysplasia detection between DCE and VCE, making VCE a viable alternative to DCE when DCE is not available. Based on a subgroup analysis including AFI, significantly higher dysplasia was detected via DCE. Thus, the results of this meta-analysis do not support AFI as an alternative to DCE in dysplasia detection in IBD. Further research is needed into the long-term outcomes of various screening modalities, including cancer and cancer-related death.
Figure: Figure 1: Forest plot summarizing the odds of dysplasia detection between dye chromoendoscopy (DCE) and virtual chromoendoscopy (VCE) in A) all studies, B) full-text articles, and C) full-text articles excluding a study that used auto-fluorescence imaging technique.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mouhand Mohamed indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Samir Shah: Roche Information Systems – Consultant.
Mouhand F.H. Mohamed, MD, MSc1, Azizullah Beran, MD2, Khalid Ahmed, MD3, Samir A. Shah, MD4. P2617 - No Differences in Dysplasia Detection Between Dye and Virtual Chromoendoscopy Techniques: Results From a Meta-Analysis of Randomized Clinical Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
