Monday Poster Session
Category: IBD
P2620 - Efficacy and Safety of Endoscopic Balloon Dilatation for Ileal Pouch-Anal Anastomosis Strictures: A Systematic Review And Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Dushyant S. Dahiya, MD
The University of Kansas School of Medicine
Kansas City, KS
Presenting Author(s)
Dushyant S. Dahiya, MD1, Anuraag Jena, MBBS2, Jay Bapaye, MD3, Babu Mohan, MD4, Lena Kassab, MD5, Antonio Facciorusso, MD, PhD6, Saurabh Chandan, MD7, Gursimran S. Kochhar, MD8
1The University of Kansas School of Medicine, Kansas City, KS; 2Postgraduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India; 3Virginia Tech Carilion School of Medicine, Roanoke, VA; 4Orlando Gastroenterology PA, Orlando, FL; 5Mayo Clinic, Rochester, MN; 6University of Foggia, Foggia, Puglia, Italy; 7CHI Health Creighton University Medical Center, Omaha, NE; 8Allegheny General Hospital, Pittsburgh, PA
Introduction: For patients with refractory inflammatory bowel disease (IBD), restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the treatment of choice. In this systematic review and meta-analysis, we assess the efficacy and safety of endoscopic balloon dilatation (EBD) for IPAA strictures.
Methods: A systematic search of numerous databases was performed through December 2023 to identify studies reporting on the outcomes of EBD in pouch-related strictures. Outcomes included technical success, clinical success at index dilation and in pouch retention, recurrence of symptoms post-EBD and adverse events of EBD. Meta-analysis was performed using a random-effects model and results were expressed in terms of pooled rates along with relevant 95% confidence intervals (CI). Heterogeneity was assessed using Cochran Q statistical test with I2 statistics.
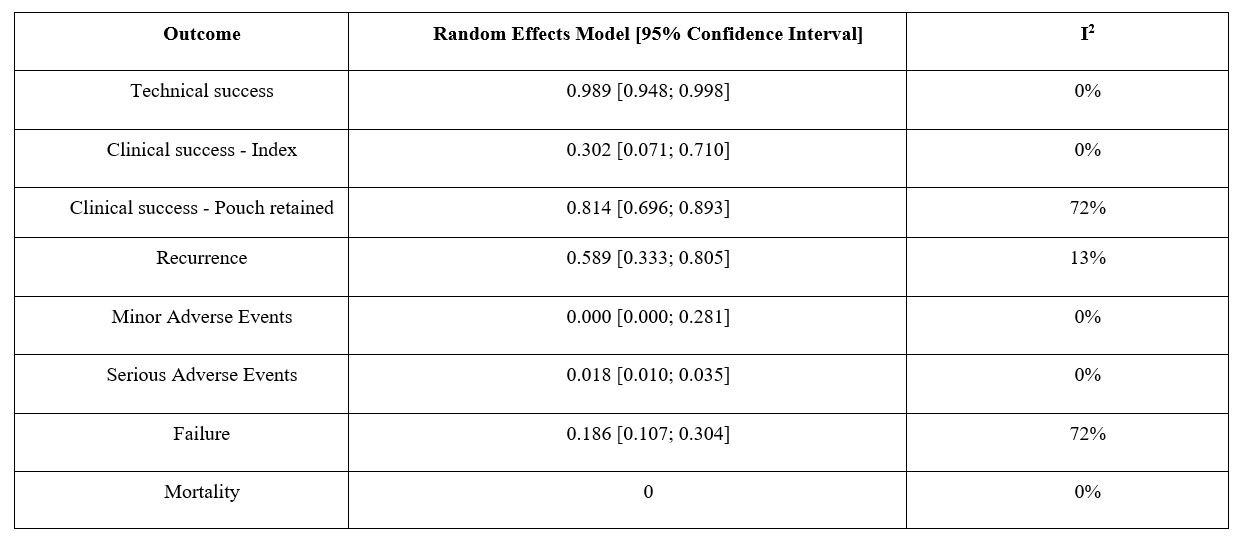
Results: Seven studies with 504 patients were included. The pooled rate of technical success, defined as the proportion of patients who had successful passage of endoscope post-dilation without resistance, and clinical success, defined as the proportion of patients who had symptomatic improvement without the need for additional dilatation, of index dilatation was 98.9% (95% CI: 94.8-99.8%; I20%) and 30.2% (95% CI: 7.1-71%; I20%), respectively.
The pooled rate of clinical success in pouch retention without the need for additional surgery (pouch excision or redo pouch) was 81.4% (95% CI: 69.6-89.3%; I272%). The pooled failure rate of EBD, defined as the proportion of patients who had permanent pouch diversion, failure of pouch retention, and/or the need for additional surgical intervention (pouch excision or redo pouch) was 18.6% (95% CI: 10.7-30.4%, I272%).
The pooled rate of recurrence of symptoms after index dilatation was 58.9% (95% CI: 33.3-80.5%; I213%). The pooled rate of serious adverse events was 1.8% (95% CI: 1-3.5%, I20%). No deaths related to EBD were reported. Figure 1 demonstrates outcomes and safety of EBD for IPAA strictures.
Discussion: EBD is safe and highly effective for management of IPAA strictures. Additional studies are needed to compare its efficacy with surgical interventions.
Disclosures:
Dushyant S. Dahiya, MD1, Anuraag Jena, MBBS2, Jay Bapaye, MD3, Babu Mohan, MD4, Lena Kassab, MD5, Antonio Facciorusso, MD, PhD6, Saurabh Chandan, MD7, Gursimran S. Kochhar, MD8. P2620 - Efficacy and Safety of Endoscopic Balloon Dilatation for Ileal Pouch-Anal Anastomosis Strictures: A Systematic Review And Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Kansas School of Medicine, Kansas City, KS; 2Postgraduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India; 3Virginia Tech Carilion School of Medicine, Roanoke, VA; 4Orlando Gastroenterology PA, Orlando, FL; 5Mayo Clinic, Rochester, MN; 6University of Foggia, Foggia, Puglia, Italy; 7CHI Health Creighton University Medical Center, Omaha, NE; 8Allegheny General Hospital, Pittsburgh, PA
Introduction: For patients with refractory inflammatory bowel disease (IBD), restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the treatment of choice. In this systematic review and meta-analysis, we assess the efficacy and safety of endoscopic balloon dilatation (EBD) for IPAA strictures.
Methods: A systematic search of numerous databases was performed through December 2023 to identify studies reporting on the outcomes of EBD in pouch-related strictures. Outcomes included technical success, clinical success at index dilation and in pouch retention, recurrence of symptoms post-EBD and adverse events of EBD. Meta-analysis was performed using a random-effects model and results were expressed in terms of pooled rates along with relevant 95% confidence intervals (CI). Heterogeneity was assessed using Cochran Q statistical test with I2 statistics.
Results: Seven studies with 504 patients were included. The pooled rate of technical success, defined as the proportion of patients who had successful passage of endoscope post-dilation without resistance, and clinical success, defined as the proportion of patients who had symptomatic improvement without the need for additional dilatation, of index dilatation was 98.9% (95% CI: 94.8-99.8%; I20%) and 30.2% (95% CI: 7.1-71%; I20%), respectively.
The pooled rate of clinical success in pouch retention without the need for additional surgery (pouch excision or redo pouch) was 81.4% (95% CI: 69.6-89.3%; I272%). The pooled failure rate of EBD, defined as the proportion of patients who had permanent pouch diversion, failure of pouch retention, and/or the need for additional surgical intervention (pouch excision or redo pouch) was 18.6% (95% CI: 10.7-30.4%, I272%).
The pooled rate of recurrence of symptoms after index dilatation was 58.9% (95% CI: 33.3-80.5%; I213%). The pooled rate of serious adverse events was 1.8% (95% CI: 1-3.5%, I20%). No deaths related to EBD were reported. Figure 1 demonstrates outcomes and safety of EBD for IPAA strictures.
Discussion: EBD is safe and highly effective for management of IPAA strictures. Additional studies are needed to compare its efficacy with surgical interventions.
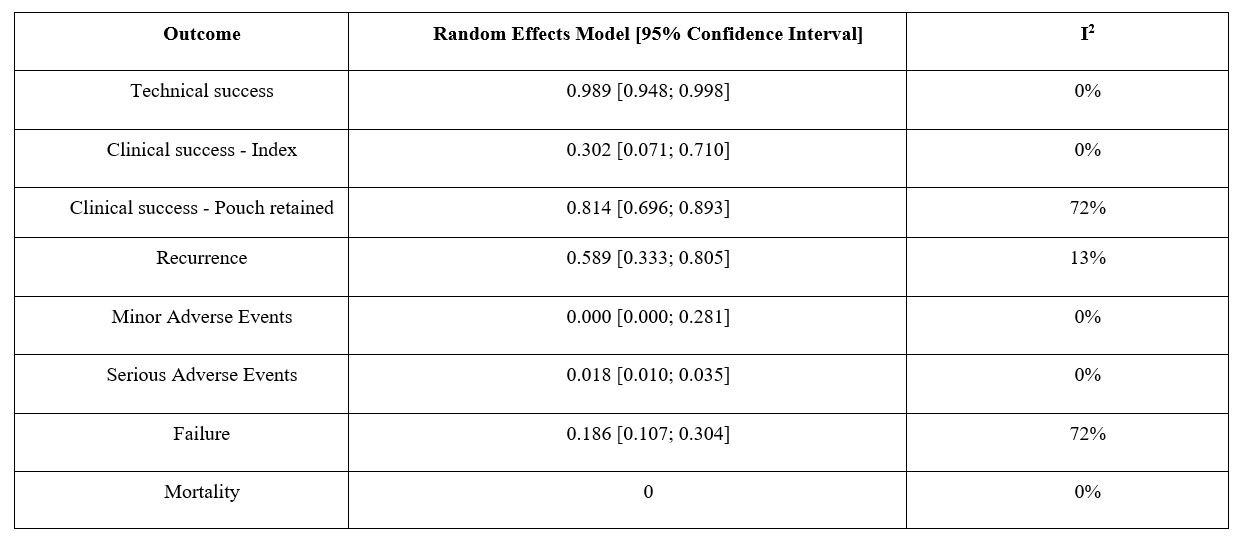
Figure: Figure1: Outcomes and safety of EBD for IPAA strictures.
Disclosures:
Dushyant Dahiya indicated no relevant financial relationships.
Anuraag Jena indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Lena Kassab indicated no relevant financial relationships.
Antonio Facciorusso indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Gursimran Kochhar: Boston Scientific Endoscopy – Consultant. DigbI – Stock Options. Eli Lilli – Advisory Committee/Board Member, Speakers Bureau. Olympus Endoscopy – Consultant. Pentax Endoscopy – Consultant. Takeda – Consultant.
Dushyant S. Dahiya, MD1, Anuraag Jena, MBBS2, Jay Bapaye, MD3, Babu Mohan, MD4, Lena Kassab, MD5, Antonio Facciorusso, MD, PhD6, Saurabh Chandan, MD7, Gursimran S. Kochhar, MD8. P2620 - Efficacy and Safety of Endoscopic Balloon Dilatation for Ileal Pouch-Anal Anastomosis Strictures: A Systematic Review And Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
