Monday Poster Session
Category: IBD
P2623 - Crohn’s Patients at Risk for Cardiovascular Complications? National Inpatient Sample Analysis Shows Concerning Outcomes
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mihir Prakash Shah, MD
John H. Stroger, Jr. Hospital of Cook County
Oklahoma City, OK
Presenting Author(s)
Mihir P. Shah, MD1, Abdulrahim Yusuf Mehadi, MD2, Rohan Gajjar, MD3, Bhanu Siva Mohan Pinnam, MD3, Daniel Guifarro, MD3, Sanket Basida, MD4, Dushyant S. Dahiya, MD5, Kajali Mishra, MD6
1John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 2John H. Stroger Hospital of Cook County, Chicago, IL; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4University of Missouri School of Medicine, Columbia, MO; 5University of Kansas Medical Center, Kansas City, KS; 6Cook County Health and Hospital Systems, Chicago, IL
Introduction: Coronary heart disease is a leading cause of morbidity and mortality in the US. Patients with Inflammatory Bowel Disease (IBD) are at increased risk for cardiovascular disease per recent reports We sought to assess the impact of Crohn’s disease on outcomes of patients admitted with NSTEMI.
Methods: A retrospective cohort study was conducted using the National Inpatient Sample (NIS) database from 2016 to 2021. All adult patients admitted due to NSTEMI were identified and were further stratified based on the presence or absence of Crohn’s disease. Patients with diseases that are known to increase cardiovascular risk (coronavirus-19, systemic lupus erythematosus, rheumatoid arthritis, systemic sclerosis, ankylosing spondylitis, psoriasis, and human immunodeficiency virus infection) were excluded from the analysis. Diseases associated with anticoagulation (atrial fibrillation/flutter, prosthetic/mechanical heart valve, intracardiac thrombus, venous thromboembolism, and hypercoagulable states) were balanced between the groups. Mortality and other in-hospital outcomes were compared between the groups, using multivariate regression to adjust for confounders.
Results: There were 4.2 million hospitalizations for NSTEMI, of which 12,740 had Crohn’s disease. Patients with Crohn’s disease were more likely to be young, female, and of Caucasian race. They were less likely to have concomitant metabolic risk factors while being more likely to have a history of venous thromboembolism.
There was no difference in overall mortality or major cardiac outcomes in Crohn’s patients compared to those without Crohn’s. However, higher odds of sepsis (OR 1.29) and gastrointestinal (GI) bleeding (OR 1.86) were noted in patients with Crohn's disease.
Discussion: Notably, mortality and cardiac outcomes were similar in the Crohn's cohort despite having a significantly lower prevalence of traditional cardiovascular risk factors (like diabetes mellitus, hypertension, and obesity). Increased GI bleeding in patients with Crohn's has significant implications for anticoagulation and antiplatelet therapy in the treatment of NSTEMI. Higher rates of sepsis can complicate the outcome, more so if patients are on immunosuppressive therapies. Physicians should be cognizant of these findings while managing patients with Crohn’s disease who present with NSTEMI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mihir P. Shah, MD1, Abdulrahim Yusuf Mehadi, MD2, Rohan Gajjar, MD3, Bhanu Siva Mohan Pinnam, MD3, Daniel Guifarro, MD3, Sanket Basida, MD4, Dushyant S. Dahiya, MD5, Kajali Mishra, MD6. P2623 - Crohn’s Patients at Risk for Cardiovascular Complications? National Inpatient Sample Analysis Shows Concerning Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 2John H. Stroger Hospital of Cook County, Chicago, IL; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4University of Missouri School of Medicine, Columbia, MO; 5University of Kansas Medical Center, Kansas City, KS; 6Cook County Health and Hospital Systems, Chicago, IL
Introduction: Coronary heart disease is a leading cause of morbidity and mortality in the US. Patients with Inflammatory Bowel Disease (IBD) are at increased risk for cardiovascular disease per recent reports We sought to assess the impact of Crohn’s disease on outcomes of patients admitted with NSTEMI.
Methods: A retrospective cohort study was conducted using the National Inpatient Sample (NIS) database from 2016 to 2021. All adult patients admitted due to NSTEMI were identified and were further stratified based on the presence or absence of Crohn’s disease. Patients with diseases that are known to increase cardiovascular risk (coronavirus-19, systemic lupus erythematosus, rheumatoid arthritis, systemic sclerosis, ankylosing spondylitis, psoriasis, and human immunodeficiency virus infection) were excluded from the analysis. Diseases associated with anticoagulation (atrial fibrillation/flutter, prosthetic/mechanical heart valve, intracardiac thrombus, venous thromboembolism, and hypercoagulable states) were balanced between the groups. Mortality and other in-hospital outcomes were compared between the groups, using multivariate regression to adjust for confounders.
Results: There were 4.2 million hospitalizations for NSTEMI, of which 12,740 had Crohn’s disease. Patients with Crohn’s disease were more likely to be young, female, and of Caucasian race. They were less likely to have concomitant metabolic risk factors while being more likely to have a history of venous thromboembolism.
There was no difference in overall mortality or major cardiac outcomes in Crohn’s patients compared to those without Crohn’s. However, higher odds of sepsis (OR 1.29) and gastrointestinal (GI) bleeding (OR 1.86) were noted in patients with Crohn's disease.
Discussion: Notably, mortality and cardiac outcomes were similar in the Crohn's cohort despite having a significantly lower prevalence of traditional cardiovascular risk factors (like diabetes mellitus, hypertension, and obesity). Increased GI bleeding in patients with Crohn's has significant implications for anticoagulation and antiplatelet therapy in the treatment of NSTEMI. Higher rates of sepsis can complicate the outcome, more so if patients are on immunosuppressive therapies. Physicians should be cognizant of these findings while managing patients with Crohn’s disease who present with NSTEMI.
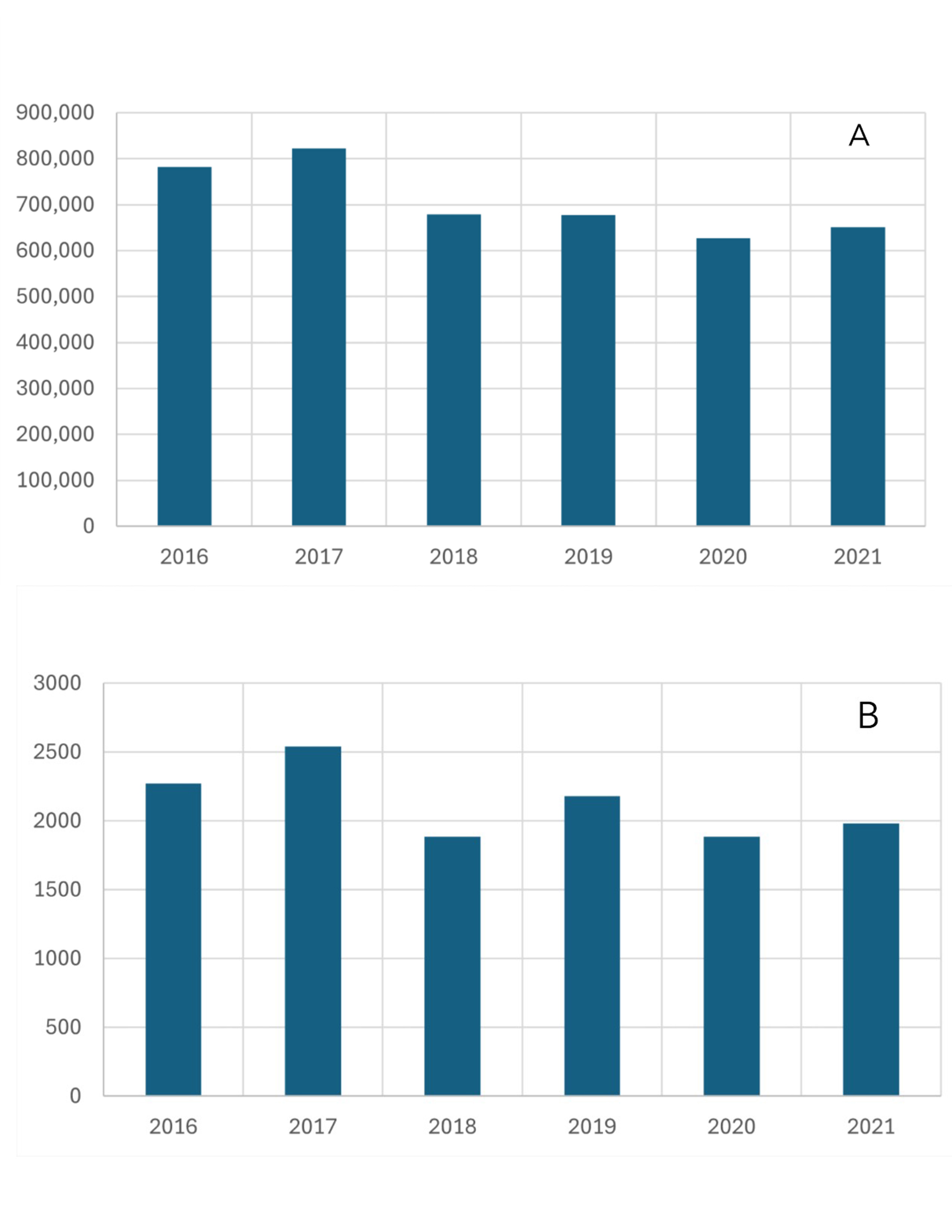
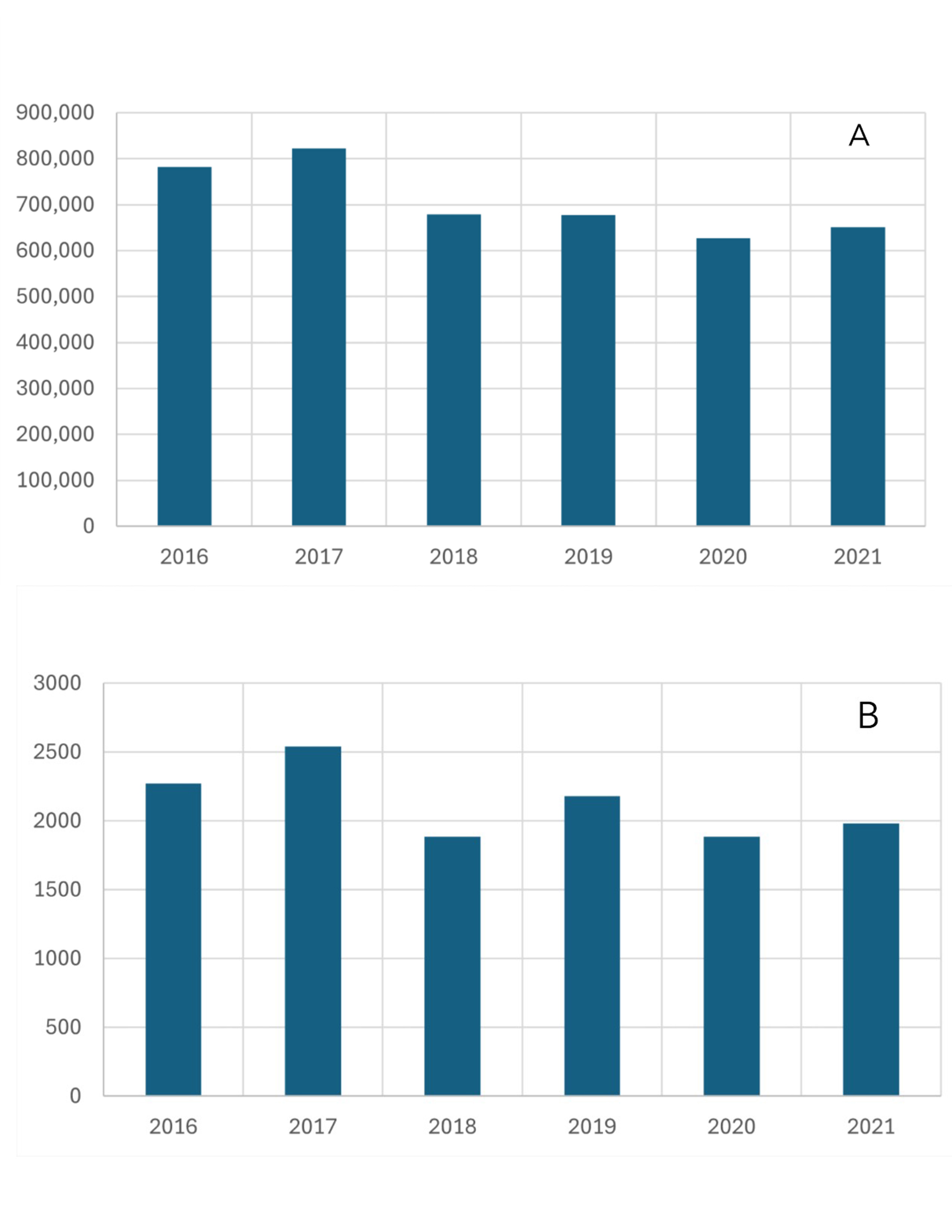
Figure: A- NSTEMI hospitalizations from 2016 to 2021
B- Crohn's disease in NSTEMI hospitalizations from 2016 to 2021
B- Crohn's disease in NSTEMI hospitalizations from 2016 to 2021
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mihir Shah indicated no relevant financial relationships.
Abdulrahim Yusuf Mehadi indicated no relevant financial relationships.
Rohan Gajjar indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Daniel Guifarro indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Kajali Mishra indicated no relevant financial relationships.
Mihir P. Shah, MD1, Abdulrahim Yusuf Mehadi, MD2, Rohan Gajjar, MD3, Bhanu Siva Mohan Pinnam, MD3, Daniel Guifarro, MD3, Sanket Basida, MD4, Dushyant S. Dahiya, MD5, Kajali Mishra, MD6. P2623 - Crohn’s Patients at Risk for Cardiovascular Complications? National Inpatient Sample Analysis Shows Concerning Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
