Monday Poster Session
Category: IBD
P2626 - The Trend of Hospitalization Outcomes for Patients With Ulcerative Colitis in the United States: 8 Year Analysis for the National Inpatient Sample
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AE
Abdelwahap Elghezewi, MBBCh
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Mohammed El-Dallal, MD, MMSc1, Jessica Crislip, MD1, Abdelwahap Elghezewi, MBBCh2, Yasmeen Obeidat, MD2, Ahmed Sherif, MD2
1Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction:
Advancements in ulcerative colitis (UC) management, including biological medications and educational initiatives, have transformed treatment. Despite this, the impact on hospitalized UC patients' outcomes remains uncertain. This study examines trends and effects on hospitalization outcomes among UC patients.
Methods: The national inpatient sample (2011-2018) was used, employing ICD codes 9 and 10 to identify UC patients, comorbidities, colonoscopies, and surgeries. Outcomes included mortality rates, hospital stay length, inflation-adjusted hospital charges, inpatient colonoscopy frequency, time to colonoscopy, adherence to a 48-hour colonoscopy window post-admission, and IBD-related surgeries. Survey methods analysis addressed sampling, with 2011 as a reference for trends in patient outcomes.
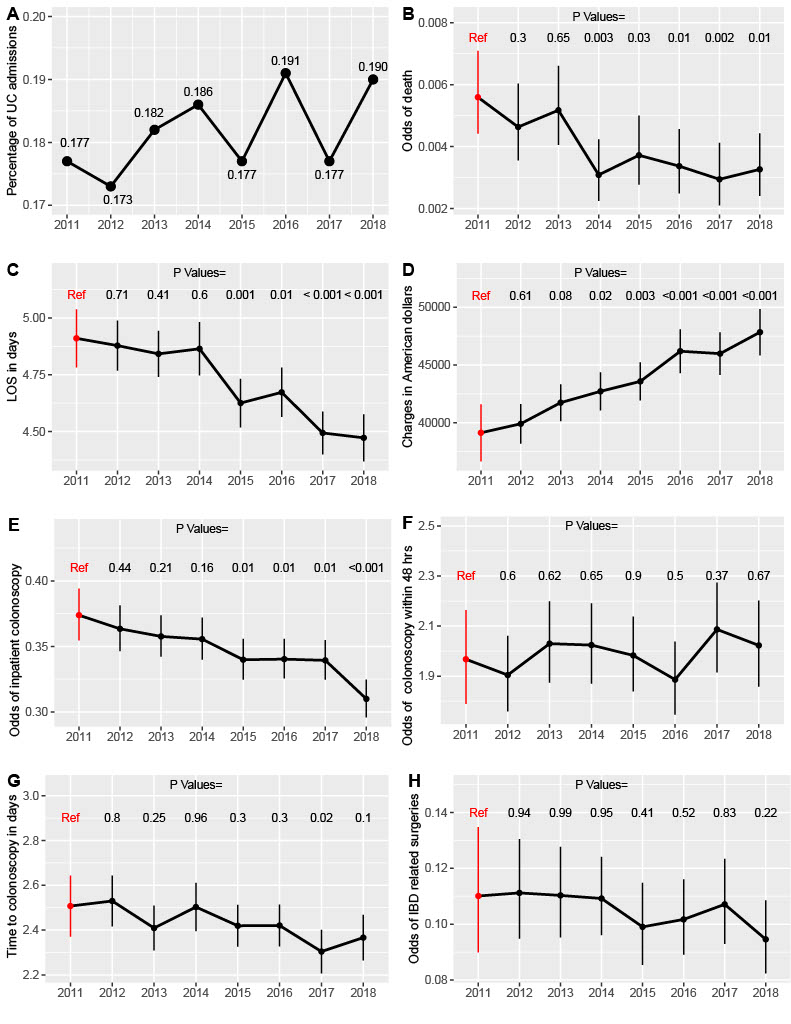
Results: In our study, comprising a weighted sample of 497,844 eligible patients from 2011 to 2018, annual distribution ranged from 59,665 to 64,909 patients, constituting 0.17% to 0.19% of total yearly hospital admissions. Table 1 presents an overview of patient and hospital characteristics. Analyzing outcomes revealed a statistically significant decline in mortality odds from 2014 onward compared to the reference year 2011, albeit with a minimal effect size (Figure 1B). Furthermore, the average length of hospital stay exhibited a gradual reduction from 2015 onwards (Figure 1C), while hospital charges increased, reaching statistical significance from 2014 to 2018 relative to 2011 (Figure 1D). The odds of inpatient colonoscopy decreased over the years, notably from 2015 to 2018 (Figure 1E). There were no significant variations in time to colonoscopy from admission, the probability of undergoing colonoscopy within 48 hours post-admission, and the frequency of IBD-related surgeries across years (Figure 1F, G, and H).
Discussion: Our study from 2011 to 2018 highlights trends in UC hospitalization outcomes. While hospitalization rates remained steady, declines in mortality and hospital stay length suggest advancements in care. The increase in hospital charges reflects UC management complexity. Diminishing inpatient colonoscopy odds indicate a shift in diagnostics. While some parameters did not exhibit statistically significant variations, our overall findings provide valuable insights into the evolving landscape of UC patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mohammed El-Dallal, MD, MMSc1, Jessica Crislip, MD1, Abdelwahap Elghezewi, MBBCh2, Yasmeen Obeidat, MD2, Ahmed Sherif, MD2. P2626 - The Trend of Hospitalization Outcomes for Patients With Ulcerative Colitis in the United States: 8 Year Analysis for the National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction:
Advancements in ulcerative colitis (UC) management, including biological medications and educational initiatives, have transformed treatment. Despite this, the impact on hospitalized UC patients' outcomes remains uncertain. This study examines trends and effects on hospitalization outcomes among UC patients.
Methods: The national inpatient sample (2011-2018) was used, employing ICD codes 9 and 10 to identify UC patients, comorbidities, colonoscopies, and surgeries. Outcomes included mortality rates, hospital stay length, inflation-adjusted hospital charges, inpatient colonoscopy frequency, time to colonoscopy, adherence to a 48-hour colonoscopy window post-admission, and IBD-related surgeries. Survey methods analysis addressed sampling, with 2011 as a reference for trends in patient outcomes.
Results: In our study, comprising a weighted sample of 497,844 eligible patients from 2011 to 2018, annual distribution ranged from 59,665 to 64,909 patients, constituting 0.17% to 0.19% of total yearly hospital admissions. Table 1 presents an overview of patient and hospital characteristics. Analyzing outcomes revealed a statistically significant decline in mortality odds from 2014 onward compared to the reference year 2011, albeit with a minimal effect size (Figure 1B). Furthermore, the average length of hospital stay exhibited a gradual reduction from 2015 onwards (Figure 1C), while hospital charges increased, reaching statistical significance from 2014 to 2018 relative to 2011 (Figure 1D). The odds of inpatient colonoscopy decreased over the years, notably from 2015 to 2018 (Figure 1E). There were no significant variations in time to colonoscopy from admission, the probability of undergoing colonoscopy within 48 hours post-admission, and the frequency of IBD-related surgeries across years (Figure 1F, G, and H).
Discussion: Our study from 2011 to 2018 highlights trends in UC hospitalization outcomes. While hospitalization rates remained steady, declines in mortality and hospital stay length suggest advancements in care. The increase in hospital charges reflects UC management complexity. Diminishing inpatient colonoscopy odds indicate a shift in diagnostics. While some parameters did not exhibit statistically significant variations, our overall findings provide valuable insights into the evolving landscape of UC patient outcomes.
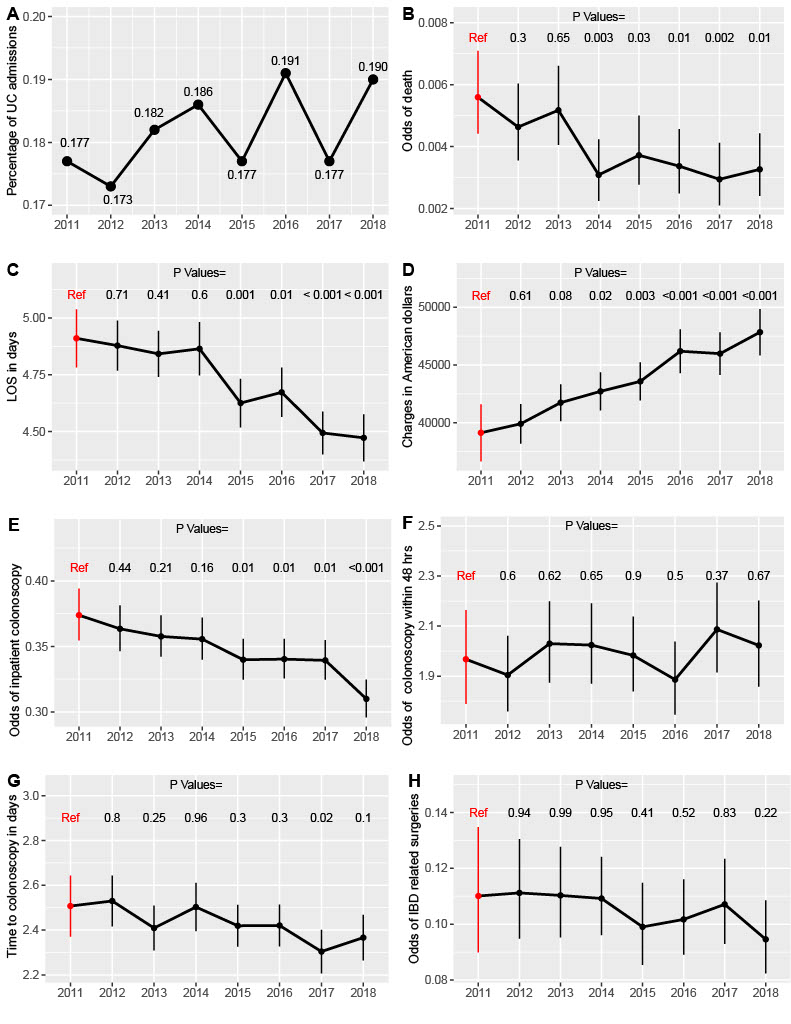
Figure: Figure 1. The trend in the hospitalization outcomes for patients admitted with primarily with ulcerative colitis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mohammed El-Dallal indicated no relevant financial relationships.
Jessica Crislip indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Mohammed El-Dallal, MD, MMSc1, Jessica Crislip, MD1, Abdelwahap Elghezewi, MBBCh2, Yasmeen Obeidat, MD2, Ahmed Sherif, MD2. P2626 - The Trend of Hospitalization Outcomes for Patients With Ulcerative Colitis in the United States: 8 Year Analysis for the National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
