Monday Poster Session
Category: IBD
P2627 - Thrombotic Events Among Hospitalized Patients With Inflammatory Bowel Disease, 2016 Through 2020
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zeinab Bakhshizarrinabadi, MD
St. Luke's Hospital
St. Louis, MO
Presenting Author(s)
Zeinab Bakhshizarrinabadi, MD1, Endurance Evbayekha, MD1, Edward V. Loftus, MD, FACG2
1St. Luke's Hospital, St. Louis, MO; 2Mayo Clinic College of Medicine and Science, Rochester, MN
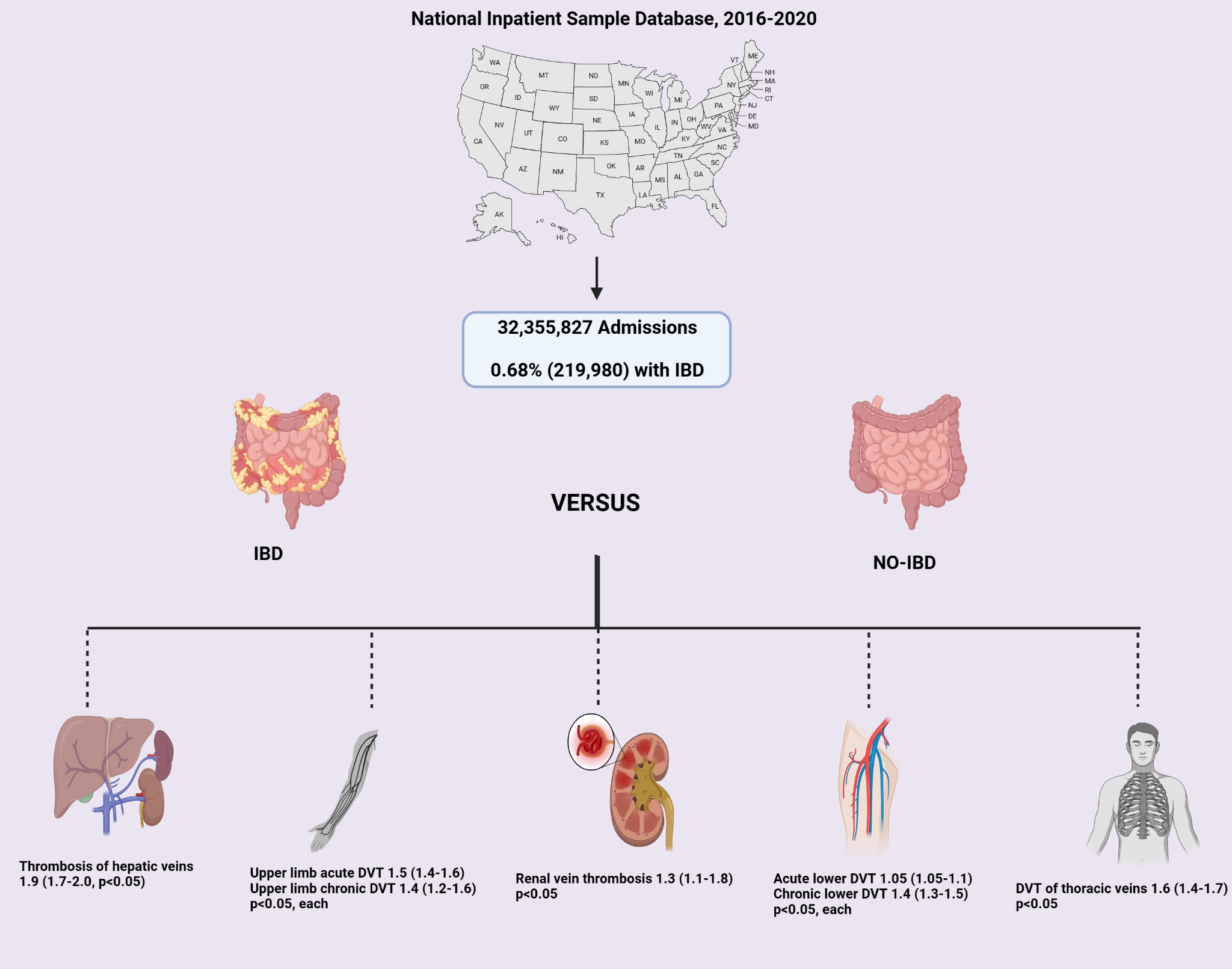
Introduction: Thrombosis is more prevalent in patients with inflammatory bowel disease (IBD) compared to the general population, yet the specific factors remain unclear. We aimed to study the association between IBD and thrombosis in various systems and to identify predictors of thrombosis in this group.
Methods: This retrospective cohort study utilized the National Inpatient Sample (NIS) data from 2016 to 2020. ICD-10 codes identified individuals >18 years old diagnosed with IBD. Disease severity was defined by having more than four active problems during hospitalization. Patients with a diagnosis of thrombotic events, including acute and chronic upper and lower limb venous thrombosis, renal, hepatic and thoracic veins thrombosis were identified using ICD-10 codes. These patients were categorized into IBD and non-IBD groups. Chi-square and Student T-test were used to compare categorical and continuous variables among IBD and non-IBD groups, and odds ratio (OR) with 95% confidence interval (95% CI) was reported. A p< 0.05 was the threshold for statistical significance. Variables with significant p-values were entered into multivariate regression, adjusting for patient and hospital-level confounders to predict the outcomes of interest.
Results: Out of the 32,355,827 admissions recorded during the study period, 0.68% (219,980) were identified with a diagnosis of IBD. The mean age for patients with IBD was 51.3 years (SD ±20), and 57% were females. The majority of these patients were White (78%), followed by Black (12.3%), Hispanic (6%), and Asian (1.1%). The hospitalization rate for IBD was 65 per 10,000 admissions in 2016 and rose modestly to approximately 70 per 10,000 in 2020 (p< 0.0001). The IBD group also had a higher cost of hospitalization, $57,422 vs $53,528 (p< 0.0001).
Compared to non-IBD patients, the IBD group had a higher likelihood of upper limb acute DVT, upper limb chronic DVT, DVT of thoracic veins, thrombosis of hepatic vein, renal vein thrombosis, acute lower DVT, and chronic lower DVT, (p< 0.05, each)Figure-1.
In the IBD group, disease severity (OR, 3.5; 95% CI, 3.4-3.6), male sex (OR, 1.3; 95% CI, 1.3-1.4), high median household income (OR, 1.1; 95% CI, 1.09-1.2), and smoking (OR, 1.2; 95% CI, 1.2-1.3) were identified as independent predictors of thrombosis (p < 0.05 for each).
Discussion: Our analysis suggests a significant association between IBD and thrombosis. Risk stratification and close monitoring in the at-risk group may improve outcomes.
Disclosures:
Zeinab Bakhshizarrinabadi, MD1, Endurance Evbayekha, MD1, Edward V. Loftus, MD, FACG2. P2627 - Thrombotic Events Among Hospitalized Patients With Inflammatory Bowel Disease, 2016 Through 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's Hospital, St. Louis, MO; 2Mayo Clinic College of Medicine and Science, Rochester, MN
Introduction: Thrombosis is more prevalent in patients with inflammatory bowel disease (IBD) compared to the general population, yet the specific factors remain unclear. We aimed to study the association between IBD and thrombosis in various systems and to identify predictors of thrombosis in this group.
Methods: This retrospective cohort study utilized the National Inpatient Sample (NIS) data from 2016 to 2020. ICD-10 codes identified individuals >18 years old diagnosed with IBD. Disease severity was defined by having more than four active problems during hospitalization. Patients with a diagnosis of thrombotic events, including acute and chronic upper and lower limb venous thrombosis, renal, hepatic and thoracic veins thrombosis were identified using ICD-10 codes. These patients were categorized into IBD and non-IBD groups. Chi-square and Student T-test were used to compare categorical and continuous variables among IBD and non-IBD groups, and odds ratio (OR) with 95% confidence interval (95% CI) was reported. A p< 0.05 was the threshold for statistical significance. Variables with significant p-values were entered into multivariate regression, adjusting for patient and hospital-level confounders to predict the outcomes of interest.
Results: Out of the 32,355,827 admissions recorded during the study period, 0.68% (219,980) were identified with a diagnosis of IBD. The mean age for patients with IBD was 51.3 years (SD ±20), and 57% were females. The majority of these patients were White (78%), followed by Black (12.3%), Hispanic (6%), and Asian (1.1%). The hospitalization rate for IBD was 65 per 10,000 admissions in 2016 and rose modestly to approximately 70 per 10,000 in 2020 (p< 0.0001). The IBD group also had a higher cost of hospitalization, $57,422 vs $53,528 (p< 0.0001).
Compared to non-IBD patients, the IBD group had a higher likelihood of upper limb acute DVT, upper limb chronic DVT, DVT of thoracic veins, thrombosis of hepatic vein, renal vein thrombosis, acute lower DVT, and chronic lower DVT, (p< 0.05, each)Figure-1.
In the IBD group, disease severity (OR, 3.5; 95% CI, 3.4-3.6), male sex (OR, 1.3; 95% CI, 1.3-1.4), high median household income (OR, 1.1; 95% CI, 1.09-1.2), and smoking (OR, 1.2; 95% CI, 1.2-1.3) were identified as independent predictors of thrombosis (p < 0.05 for each).
Discussion: Our analysis suggests a significant association between IBD and thrombosis. Risk stratification and close monitoring in the at-risk group may improve outcomes.
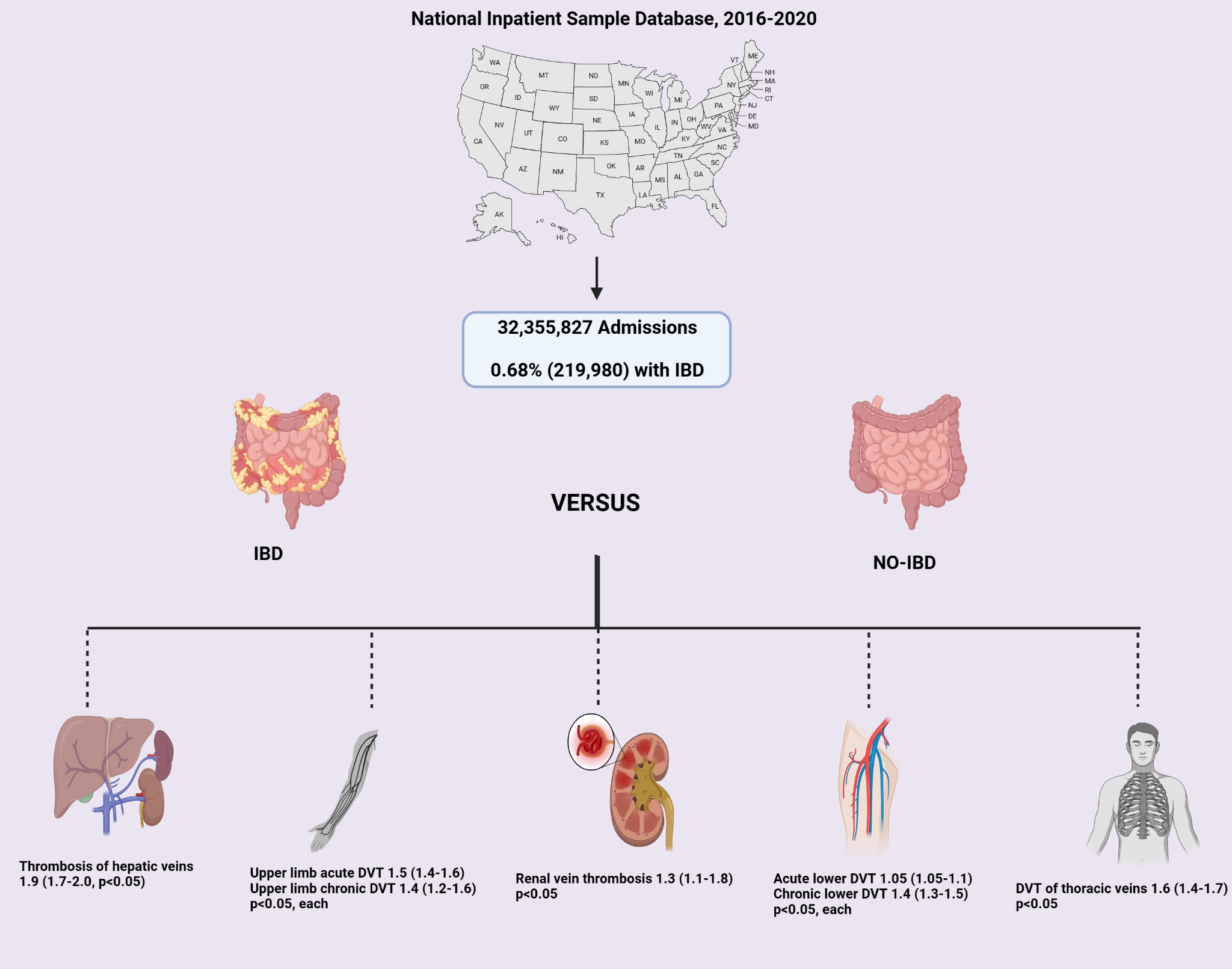
Figure: The likelihood of thrombotic events among patients with IBD vs patients without IBD
Disclosures:
Zeinab Bakhshizarrinabadi indicated no relevant financial relationships.
Endurance Evbayekha indicated no relevant financial relationships.
Edward Loftus: AbbVie – Consultant, Grant/Research Support. Amgen – Consultant. Astellas – Consultant. AstraZeneca – Grant/Research Support. Avalo – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support. Celgene – Consultant. Celltrion – Consultant. Eli Lilly – Consultant. Exact Sciences – Stock-publicly held company(excluding mutual/index funds). Fresenius Kabi – Consultant. Genentech – Consultant, Grant/Research Support. Gilead – Consultant, Grant/Research Support. Iota Biosciences – Consultant. Iterative Health – Grant/Research Support. Janssen – Consultant, Grant/Research Support. Merck – Consultant. Morphic Therapeutics – Consultant. Ono Pharma – Consultant. Receptos – Grant/Research Support. Sun Pharma – Consultant. Surrozen – Consultant. Takeda – Consultant, Grant/Research Support. TR1X Bio – Consultant. UCB – Consultant, Grant/Research Support.
Zeinab Bakhshizarrinabadi, MD1, Endurance Evbayekha, MD1, Edward V. Loftus, MD, FACG2. P2627 - Thrombotic Events Among Hospitalized Patients With Inflammatory Bowel Disease, 2016 Through 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
