Monday Poster Session
Category: IBD
P2551 - Higher Incidence of Recombinant Zoster Vaccination in Patients With Inflammatory Bowel Disease: A TriNetX Database Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Yichen Wang, MD
University of Pennsylvania
Philadelphia, PA
Presenting Author(s)
Yichen Wang, MD1, Yuting Huang, MBBS, PhD2, Aakash Desai, MD3, Jana G. Hashash, MD, MSc2, Freddy Caldera, DO, PhD4, Francis A. Farraye, MD, MSc2
1University of Pennsylvania, Philadelphia, PA; 2Mayo Clinic, Jacksonville, FL; 3Mayo Clinic, Pittsburgh, PA; 4University of Wisconsin School of Medicine and Public Health, MIddleton, WI
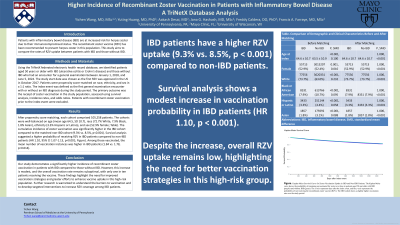
Introduction: Patients with inflammatory bowel disease (IBD) are at increased risk for herpes zoster due to their underlying disease and drug-associated immunosuppression. The recombinant zoster vaccine (RZV) has been recommended to prevent herpes zoster in this population. This study aims to compare the rates of RZV uptake between patients with IBD and those without IBD.
Methods: Using TriNetX, a multi-institutional US database, we identified patients aged 50 years or older with IBD (ulcerative colitis or Crohn's disease) and those without IBD who had an encounter for a general examination between January 1, 2018, and June 5, 2024. The study start date was chosen as RZV was approved in the US in October 2017. Patients were propensity score-matched on race, ethnicity, and sex in a 1:1 ratio. The index event was defined as the first general examination encounter with or without an IBD diagnosis during the study period. The primary outcome was the receipt of RZV in the study population, assessed using survival analysis, incidence rates, and odds ratios. Patients with recombinant zoster vaccination prior to the index event were excluded.
Results: After propensity score matching, each cohort comprised 105,258 patients. The cohorts were well-balanced on age (mean age 64.5, SD 10.7), race (72.7% White, 7.9% Black, 1.8% Asian), ethnicity (3.3% Hispanic or Latino), and sex (52.9% female; Table). The cumulative incidence of zoster vaccination was significantly higher in the IBD cohort compared to the matched non-IBD cohort (9.3% vs. 8.5%, p< 0.001). Survival analysis suggested a higher probability of receiving RZV in patients with IBD compared to non-IBD patients (HR 1.10, 95% CI 1.07-1.13, p< 0.001; Figure). Among those vaccinated, the mean number of vaccine administrations was higher in IBD patients (1.84 vs. 1.78, p=0.014).
Discussion: Our study demonstrates a significantly higher incidence of recombinant zoster vaccination in patients with IBD compared to those without IBD. However, this increase is modest, and the overall vaccination rate remains suboptimal, with only one in ten patients receiving the vaccine. These findings highlight the need for improved vaccination strategies and greater efforts to enhance vaccine uptake in this high-risk population. Further research is warranted to understand the barriers to vaccination and to develop targeted interventions to increase RZV coverage among patients with IBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yichen Wang, MD1, Yuting Huang, MBBS, PhD2, Aakash Desai, MD3, Jana G. Hashash, MD, MSc2, Freddy Caldera, DO, PhD4, Francis A. Farraye, MD, MSc2. P2551 - Higher Incidence of Recombinant Zoster Vaccination in Patients With Inflammatory Bowel Disease: A TriNetX Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pennsylvania, Philadelphia, PA; 2Mayo Clinic, Jacksonville, FL; 3Mayo Clinic, Pittsburgh, PA; 4University of Wisconsin School of Medicine and Public Health, MIddleton, WI
Introduction: Patients with inflammatory bowel disease (IBD) are at increased risk for herpes zoster due to their underlying disease and drug-associated immunosuppression. The recombinant zoster vaccine (RZV) has been recommended to prevent herpes zoster in this population. This study aims to compare the rates of RZV uptake between patients with IBD and those without IBD.
Methods: Using TriNetX, a multi-institutional US database, we identified patients aged 50 years or older with IBD (ulcerative colitis or Crohn's disease) and those without IBD who had an encounter for a general examination between January 1, 2018, and June 5, 2024. The study start date was chosen as RZV was approved in the US in October 2017. Patients were propensity score-matched on race, ethnicity, and sex in a 1:1 ratio. The index event was defined as the first general examination encounter with or without an IBD diagnosis during the study period. The primary outcome was the receipt of RZV in the study population, assessed using survival analysis, incidence rates, and odds ratios. Patients with recombinant zoster vaccination prior to the index event were excluded.
Results: After propensity score matching, each cohort comprised 105,258 patients. The cohorts were well-balanced on age (mean age 64.5, SD 10.7), race (72.7% White, 7.9% Black, 1.8% Asian), ethnicity (3.3% Hispanic or Latino), and sex (52.9% female; Table). The cumulative incidence of zoster vaccination was significantly higher in the IBD cohort compared to the matched non-IBD cohort (9.3% vs. 8.5%, p< 0.001). Survival analysis suggested a higher probability of receiving RZV in patients with IBD compared to non-IBD patients (HR 1.10, 95% CI 1.07-1.13, p< 0.001; Figure). Among those vaccinated, the mean number of vaccine administrations was higher in IBD patients (1.84 vs. 1.78, p=0.014).
Discussion: Our study demonstrates a significantly higher incidence of recombinant zoster vaccination in patients with IBD compared to those without IBD. However, this increase is modest, and the overall vaccination rate remains suboptimal, with only one in ten patients receiving the vaccine. These findings highlight the need for improved vaccination strategies and greater efforts to enhance vaccine uptake in this high-risk population. Further research is warranted to understand the barriers to vaccination and to develop targeted interventions to increase RZV coverage among patients with IBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yichen Wang indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Jana Hashash: Bristol Myers Squibb – Consultant.
Freddy Caldera: GSK – Consultant. GSK – Grant/Research Support. Janssen – Advisory Committee/Board Member. Janssen – Consultant. Novavax – Grant/Research Support.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Yichen Wang, MD1, Yuting Huang, MBBS, PhD2, Aakash Desai, MD3, Jana G. Hashash, MD, MSc2, Freddy Caldera, DO, PhD4, Francis A. Farraye, MD, MSc2. P2551 - Higher Incidence of Recombinant Zoster Vaccination in Patients With Inflammatory Bowel Disease: A TriNetX Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
